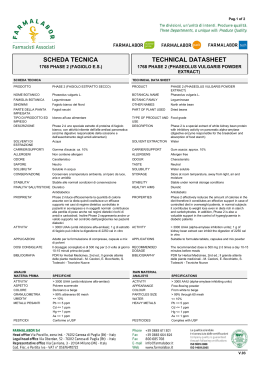
La Terapia delle Fibrosi Polmonari Venerino Poletti Ospedale GB Morgagni Forlì (I) Therapeutic Approaches to ILDs ILDs treatment is guided by: • • • • ILDs Aetiology (Known and Unknown causes) ILDs Pathology (Inflammatory and Fibrotic) Severity of disease and Disease Behaviour The clinical context (age, comorbidities, complications) An Official American Thoracic Society/European Respiratory Society Statement: Update of the International Multidisciplinary Classification of the Idiopathic Interstitial Pneumonias. Travis, Am J Respir Crit Care Med 2013 ILDs of known cause Drug induced Occupational and Environmental Exposure Collagen Vascular Diseases Associated Hypersensitivity pneumonitis (HP) is a complex syndrome of varying intensity, clinical presentation, and natural history. Several different diagnostic criteria for HP have been proposed. Most apply only to typical, acute cases. No clear diagnostic criteria exist for subacute or chronic disease. HP acute form HOURS -2 DAYS begin 2–9 h after exposure, peak during 6 and 24 h, and last from hours to days. influenza-like symptoms (chills, fever, sweating, myalgias, lassitude, headache and Nausea) Respiratory symptoms such as cough and dyspnoea are common but not universal. HP subacute form DAYS-WEEKS appear gradually over several days to weeks, cough and dyspnoea, and may progress to severe dyspnoea and cyanosis, leading to urgent hospitalization. HP chronic form MONTHS insidious onset over a period of months, increasing cough and exertional dyspnoea, fatigue , weight loss, digital clubbing. Chronic bird fancier's lung: histopathological and clinical correlation. group A BOOP-like or cellular NSIP-like lesions, n = 7; group B fibrotic NSIP-like lesions, n = 8; group C UIP-like lesions, n = 11. Chronic HP Treatment Eliminate the causal agent Prednisone 20-40 mg, tapered to 10mg/d up to 8 weeks, although fibrotic HP is less likely to respond. In chronic, progressive HP, immunosuppressants may be added as corticosteroid sparing agents, as done in other fibrotic ILD. There is no antifibrotic treatment for chronic advanced HP patients and lung transplantation should be considered. Rituximab CTD-ILDs Prognosis CTD-ILD have a better prognosis compared to IIPs. Survival of RA-UIP does NOT differ from IPF (3.5y) Park JH, AJRCCM 2007 CTD-ILDs Treatment 1) DO NOT TREAT trivial ILDs: Mild (HRCT extension <20% , DLco > 65%, FVC >75%) and stable. 2) TREATMENT FOR SLOWLY PROGRESSIVE CTD-ILDs Prednisone po 0.5-1mg/Kg tapered to a maintenace dose of 10mg/day in association with Azathioprine po 150mg/dì. Duration 2-3 years. Alternatives: -Mycophenolate po 250mg bd, up to 1000mg twice a day (seems to be better tolerated, thera are NO clinical trials) 3) SALVAGE TREATMENT: consider Rituximab 1g followed by 1g after 2 weeks (case series: Jo1+PM, SSc) MMF DOSE Daily dose of MMF 3000 mg/day in 65% In only 4 subjects was the daily dose<2000 mg. None exceeded a dose of 3000 mg/day MEDIAN DURATION of MMF USE 897 days SIDE EFFECTS/DISCONTINUATION In 13 subjects (10%) MMF was discontinuated (2 gastrointestinal intolerance, 2 ILD progression , 2 hepatic transaminase elevation, 1 recurrent infections, 1 cytopenia, 4 non specific symptoms) Idiopathic ILDs An Official American Thoracic Society/European Respiratory Society Statement: Update of the International Multidisciplinary Classification of the Idiopathic Interstitial Pneumonias. Travis, Am J Respir Crit Care Med 2013 Pirfenidone Pirfenidone: Antifibrotic, antioxidant, anti-TNF Different experimental models :heart, lung, kidney fibrosis A series of four randomized controlled studies: (>1100 patients) Pirfenidone dosage N Changes in VC decline/placebo Ref Azuma 1800 mg/d Placebo 72 35 ΔVC 100 ml (9mo) AJRCCM 2005 Taniguchi 1800 mg/d 1200 mg/d Placebo 108 55 104 ΔFVC 70 ml (12 mo) ERJ 2010 PIPF 004 2403 mg/d 1197 mg/d Placebo 174 174 87 ΔFVC =4% pred. (12% vs 8%) 72 wks Noble, Lancet 2011 PIPF 006 2403 mg/d Placebo 171 173 NS Noble, Lancet 2011 FVC decline Grouped analysis % patients with ΔFVC > 10% 2403 mg Placebo 21% 31% P 0.003 Progression free survival RR=0.74 P=0.025 Distance 6MWT Δ=24m P=0.009 Positive trend for mortality reduction (Noble, Lancet 2011;377:1760) L’uso del Pirfenidone nella pratica clinica: cosa abbiamo imparato? PROFILO POPOLAZIONE, N = 83 PAZIENTI TRATTATI maschi (68, 82%), età media 66 anni (range, 46-81). FVC del 74% del predetto (131-35), DLco 47% (89-20). EVENTI AVVERSI - avversi frequentemente osservati (43% dei pazienti) sono stati: astenia, difficoltà di concentrazione, artralgie, e perdita di peso. - sintomi gastrointestinali 34%, - rush cutaneo 20% (11% da fotosensibilità), - aumento degli enzimi epatici 3%. L’uso del Pirfenidone nella pratica clinica: cosa abbiamo imparato? - Abbiamo osservato in totale 50 eventi avversi di cui : - 6 (12%) gravi (2 aumentI enzimi epatici, 1 rash cutaneo, 1 reazione da fotosensibilità, 2 cachessia) che hanno richiesto la definitiva sospensione del farmaco. - 19 (38%) lievi e sono stati affrontati senza necessità di modificare la dose assunta. - I rimanenti 25 (50%) erano lievi-moderati e sono stati affrontati con approci diversi: riduzione della dose (5), temporanea interruzione (10) o definitiva sospensione (10). - Tutti gli eventi avversi sono stati completamente reversibili. FOLLOW-UP - 14 pazienti sono deceduti (10 di esacerbazione acuta diIPF) - 7 pazienti la malattia è progredita. 0.25 0.50 0.75 1.00 La sopravvivenza libera da progressione di malattia dopo 12 mesi di trattamento è stata del 87.03% (95% CI 77%-93%) per il Pirfenidone e del 72.05 % (95% CI 65%-78%) per I pazienti trattati con altri farmaci (p=0.0114) 0.00 N 0 Number at risk N 186 Y 83 Y 6 12 18 24 89 11 68 0 time (months) 152 73 111 35 N Engl J Med 2012;366:1968-77. Increased mortality in treated patients N Engl J Med 2012;366:1968-77. (IPFNet, NEJM 2012) Increased mortality and hospitalization rate N Engl J Med 2012;366:1968-77. (IPFNet, NEJM 2012) PANTHER trial – Is NAC effective ? NAC (600 mg x3/d) N=260 60 weeks Placebo Results expected 1q 2014 BIBF 1120 (nintedanib, Vargatef®) : multi-target Tyrosine Kinase inhibitor Triple angiokinase Inhibitor Involved in IPF pathogenesis Hilberg, Cancer Res 2008 The TOMORROW study (Richeldi, NEJM 2011;365:1079) Placebo N=85 BIBF 1120-300mg N=85 FVC 12 mo - 190 ml - 60 ml 0,013 Exacerbations 15,7 % 2,4 % 0,02 SGRQ +5,46 -0,66 0,0007 GI side effects (drug stop) Diarrhea 11,8% vs 0% Nausea 4,7% vs 0% Vomiting 2,4% vs 1,2% P value -68% Two Phase 3 trials (Inpulsis) Results expected end 2013 A non exhaustive list ot targets Anti-TGFβ Anti CTGF Anti-CCL2 Anti-IL-13 Anti-IL-4, IL-13 JNKi Anti-αvβ6 Anti LOXL2 SAP CO inhalé MMPs Anti-LTs Interferon alpha Aerosolized IFNγ Collagen V Octreotide PI3Kinase Sirolimus Serotonin, LPA1, losartan, … Fresolimumab (Sanofi-Genzyme, Phase1) FG-3019 (Fibrogen, Phase2) CNTO 888 (Phase 2) QAX-576 (Novartis, Phase 2) Tralokinumab (AZ-MedImmune, Phase 2) SAR156597 (Sanofi, Phase 2) CC-930 (Celgene, Phase 2) STX-100 (Stromedix, Phase 2) simtuzumab (Gilead, Phase 2) PRM-151 (Promedior, Phase 2) Phase 2 minocycline zileuton Phase 1 (Thorax 2011) Phase 2 IW001 (Immuneworks, Phase 1) FIBROSAND (Phase 2) ERJ 2012 GSK2126458 (GSK, Phase 1) Is bacterial Infection/colonization a target in IPF ? Apoptosis cotrimoxazole : 960mg x 2/j Folic acid: 5mg/j cotrimoxazole (Shulgina, Thorax 2012; on line First) 3/53 14/65 Survie Improvement of mortality in the per-protocol population HR: 0.21 (IC95%: 0.06-0.78) p=0.02 Others... Failure of monotargeted therapies nintedanib pirfenidone 2013 Next step ? Should we treat GERD ? Retrospective analysis of 2 IPF cohorts Prolonged survival associated with : FVC ↑ DLCO ↑ Anti-GERD Tt Lee, AJRCCM 2011 Should we treat PHT in IPF ? Specific Tts are not recommended Hoeper, Int J Cardiol 2011;154S:S45-S53 Pulmonary edema in case of veno-occlusive component Colombat, Hum Pathol 2007;38:60-65 Ambrisentan increased mortality in a recent trial Raghu (ATS 2012) Identify the right patient ? Sildenafil improves QoL and dyspnea score if RV dysfunction IPFNet, NEJM 2010;363:620-8; Han, Chest 2013, on line; Riociguat (guanylate cyclase agonist) to be evaluated Hoeper, ERJ 2012, on line Do not forget… Lung transplant is the only treatment shown to improve survival in IPF patients A treatment of exception (<3%) Evaluate patients < 65 years Be ready for exacerbation : Evaluate early rather than late DLCO<40% CVF>10% or lung function decline Egan, Thorax 2005; Wells, Interstitial Lung Disease guideline, Thorax 2008;63 Suppl 5 Raghu, AJRCCM 2011;183:788-824 Palliative Care in IPF Ravaglia C, et al. J Pall Care 2013 *This approach is recommended in IPF patients *NIV/Mechanical ventilation only in very selected cases Novel Treatments for other ILDs Established and experimental medical therapy of pulmonary sarcoidosis. Baughman RP, Nunes H, Sweiss NJ, Lower EE. Eur Respir J. 2013 Jun;41(6):1424-38. Standard treatments for pulmonary sarcoidosis, includes glucocorticoids, and cytotoxic agents, such as methotrexate, azathioprine and leflunomide, Newer biological agents, such as infliximab and adalimumab. There is, as yet, no standard assessment for response, there is a growing consensus that response to treatment may include improvement of one or more of the following: forced vital capacity, chest imaging and steroid sparing. Several drugs used for pulmonary sarcoidosis have demonstrated improvement in one or more of these measures. Recommendations can be either strong (1A, 1B, 1C) or weak (2A, 2B, 2C).
Scaricare