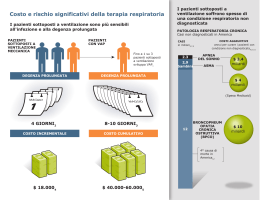
Mortality and RDI 7.0 < 59 yr > 59 yr 6.0 Log Odds 5.0 4.0 3.0 2.0 1.0 0.0 -1.0 0-10 11.-20 20-40 RDI >40 Long-term Cardiovascular Outcomes in Men with OSAS Controls n = 264 Snorers n = 377 Mild OSAH n = 403 Severe OSAH n = 235 OSAH with CPAP n = 372 JM Marin et al. Lancet 2005; 365:1046-1053 SLEEP DISORDERED BREATHING AND MORTALITY: EIGHTEEN-YEAR FOLLOW-UP OF THE WISCONSIN SLEEP COHORT YOUNG ET AL. SLEEP, VOL. 31, NO. 8, 2008 Mean age 48 yrs Marshall – Sleep 2008; 31: 1079-1085 Cardiovascular disease and mortality in OSAS patients at baseline and after 10-yr follow-up Doherty et al. Chest 2005; 127: 2076-2084 * LOW COMPLIANCE TO TREATMENT DECREASES SURVIVAL. Campos-Rodriguez et al. Chest 2005; 128: 624-633 CAMBIAMENTI DI PERSONALITÀ E DISTURBI DELL’UMORE Depressione, irascibilità o aggressività Alterazione delle funzioni psichiche superiori • D E F I C IT D E L L ’ ATT E N Z IO N E E D E L L A M E M O R I A • D I F F I C OLTÀ D I C O N C ENTRA ZIO NE • R ID OTTA A B ILITÀ M A N UALE PRO PO R ZIONALE A L N U M ERO D I APNEE NEL SONNO • S C A R S E P E R FO R M A N C E L AVO R AT IV E O D I ST U D IO P E R P RO B L E M I V I S I VI E P S I C O MOTORI ; Q U E STE A LT ERA ZI ONI S O N O D OV UTE A L L A FR A M MENTAZION E D EL S O N N O E A LLA C O N S EGUENTE IPO S SIA CEREBRALE. Table 3 – CBA 2.0 Schedule 4: answers’ frequency distributions Inquiry Area Answer n (%) Relationship with parents Good Poor 86 (67.7%) 41 (25.3%) Couple relationship Good Poor 84 (72.4%) 32 (27.6%) Sexual activity Regular/satisfactory Not regular/unsatisfactory 60 (43.5%) 78 (56.5%) Sexual disturbances No Yes 94 (50.4%) 63 (49.6%) Financial situation Good Poor 91 (53.2%) 66 (46.8%) Smoking No Yes 98 (59.0%) 59 (41.0%) Psychopharmacological treatment No Yes 144 (90.4%) 13 (9.6%) Suicidal thoughts Yes No 12 (9.1%) 145 (90.9%) Pierobon Sleep Medicine 2008 WHY WE NEED TO TREAT OSA? OSA: high prevalence of erectile dysfunction in man due to neuropathy development. Strong correlation between the severity of nerve damage and severity of nocturnal hypoxia. Fanfulla et al Sleep 2000 Riflesso bulbocavernoso in OSAS normale alterato Eccessiva sonnolenza diurna Sensazione soggettiva di un imperioso bisogno di sonno in una condizione non usuale (tempo e luogo) o episodio di addormentamento non intenzionale o in una condizione non usuale (tempo e luogo). American Sleep Disorders Association, ICSD. DRIVING, SLEEP AND ACCIDENTS Effect of time of day (p<0.001) Sleep-related accidents Traffic density Traffic Density 160 8 140 7 120 6 100 5 80 4 60 3 40 2 20 1 0 0 0 2 4 6 8 10 12 14 Time of the day 16 18 20 22 proporzionality ratio n. of sleep related accidents Relative hourly probability risk N of Sleep-Related Accidents Relative Risk of Sleep-Related Accidents “ un guidatore viene definito come sonnolento alla guida se diventa così sonnolento mentre guida da aver paura di addormentarsi e se tale severa sonnolenza durante la guida compaia almeno una volta su tre quando impegnato in un lungo tragitto autostradale”. RISK OF SLEEP APNEA IN SLEEPY DRIVERS 60 5.7 (1.3-24) 52 50 6.0 (1.1-32)10.0 (1.5-66) 42 SWD 40 40 No SWD % 30 20 17 13 9 10 0 >10 >15 >20 AHI Confounding variables: hypertension, body mass index, gender, age and snoring Masa AJRCCM 2000 Accidents risk in sleepy drivers with/without sleep apnea % of drivers with accidents 60 50 6.6 (1.1-44) 8.5 (1.2-59) 8.9 (1.3-62) 47 43 50 Sleep apnea No Sleep apnea 40 30 20 10 13 12 12 10 0 >10-<10 >15-<15 >20-<20 Drivers Control AHI Confounding variables: hypertension, drugs causing sleepiness, body mass index, gender, age, alcohol consumed, insomnia, hours slept per night, work and sleep schedule, professional drivers, hours driven per month and years of driving. SLEEP, DRIVING AND SLEEP APNEA If we turn to medical matters, a recent meta-analysis points to Obstructive Sleep Apnea as the disease resulting in the highest risks of being involved in an accident with injuries Low Risk Impairment Vision, arthritis/locomotor, Hearing, Cardiovascular Relative risk < 1.25 Medium risk impairment Diabetes Mellitus Relative risk 1.56 High Risk Impairment Alcoholism, Neurological, Mental, Drugs/Medicines Relative Risk 1.58 – 2.0 Very High Risk Sleep Apnea/Narcolepsy* Relative Risk 3.71 (only one study on Narcolepsy) Truls Vaa Impairments, Diseases, age and their relative risks of accidents involvement. Institute for Transport Economics, Oslo, Norway, 2003 A 60 Km/h in 6 secondi si percorrono 100 metri DRIVING ABILITY IN SLEEP APNOEA PATIENTS BEFORE AND AFTER CPAP TREATMENT Mazza ERJ 2006 Determinants Affecting Health-Care Utilization in Obstructive Sleep Apnea Syndrome Patients OSAS patients are heavy users of health-care resources. Age >65 years and female gender were the leading elements predicting the most costly OSAS patients, and not necessarily patients with a high BMI and classic OSAS severity indexes. This was due to higher comorbidity, ie, 10 to 30% more hypertension, ischemic heart disease, diabetes mellitus, and pulmonary disease. Ariel Tarasiuk, et al CHEST 2005; 128:1310–1314) Low Socioeconomic Status Is a Risk Factor for Cardiovascular Disease Among Adult OSAS Patients Requiring Treatment In addition to the already known traditional risk factors, low SES was found to be a novel independent risk factor for CVD among adult OSAS patients requiring treatment. Ariel Tarasiuk, et al CHEST 2006; 130:766–773) FUTURO Identificare (HTA) nuovi modelli gestionali: Rete (modello HUB – Spoke – rete assistenziale territoriale) Sistema piramidale (ambulatorio – DH – Degenza) Reti ospedaliere Modelli integrati FUTURO Cosa si chiede alla politica sanitaria: 1. Riconoscimento della specificità della medicina del sonno, compresa quella respiratoria (ICD – Nomenclatore) 2. Il riconoscimento dell’OSAS come malattia sociale 3. Escludere la CPAP dalla disciplina protesica CONCLUSIONI Fare in modo che il futuro da “minaccia” diventi promessa (o opportunità).
Scaricare