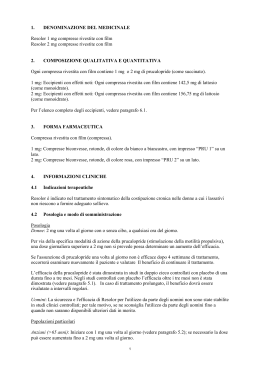
Fondazione Rosa Gallo “Attualità chirurgiche nelle malattie del colon-retto” Verona, 14 giugno 2012 Simposio “La stipsi severa attualità terapeutiche” “Novità nella terapia medica” Gabriele Riegler Seconda Università di Napoli STIPSI E LASSATIVI CAMPIONE INTERVISTATO ETA’ 20 - 40 41 - 60 >60 Riegler G. et al.: Clin. Ter. 1986 M. F. TOT. 403 408 811 213 113 77 159 138 111 372 251 188 STIPSI E LASSATIVI 330/811 (40.7%) ASSUMEVANO LASSATIVI Riegler G. et al.: Clin. Ter. 1986 STIPSI E LASSATIVI USO DEI LASSATIVI ASSUNZIONE VS.PRESCRIZIONE ASSUNZIONE SETTIMANALE 3-7 VOLTE 1-2 “ <1 “ Riegler G. et al.: Clin. Ter. 1986 PRESCRITTI SI NO 67% 52% 29% 33% 48% 71% STIPSI E LASSATIVI EFFICACIA TERAPEUTICA BUONA MEDIOCRE NULLA 58% 14% 28% EFFETTI COLLATERALI 14% Riegler G. et al.: Clin. Ter. 1986 STIPSI E LASSATIVI CATEGORIE DI FARMACI • DA CONTATTO • OSMOTICI • DETERGENTI • LUBRIFICANTI • FIBRE Riegler G. et al.: Clin. Ter. 1986 57% 36% 28% 16% 4% 229 pazienti con stipsi funzionale: terapie Consigli dietetici Fibre Lassativi Clistere Supposte Probiotici Antispastici Antidepressivi Ansiolitici Antibiotici intestinali Psicoterapia Riabilitazione pav.pelvi 0 Bellini M. et al. 20 40 60 80 100 % FIBRE IDROSOLUBILI • PHGG • FOS • INULINA • GUAR • PSYLLIUM • ALGINATI • PECTINA FIBRE NON IDROSOLUBILI • EMICELLULOSA • CELLULOSA • LIGNINA MECCANISMO D’AZIONE DELLE FIBRE insolubili solubili < svuotamento gastrico + < transito tenue + > transito tenue + > transito colon + < assorbimento + < assorbimento colesterolo + > peso & volume feci + + > fermentazione + ++ > acidi grassi a catena corta ++ + Effect of fibre on global symptom improvement SOLUBLE FIBRE Arthurs and Fielding, 1983 Jalihal and Kurian, 1999 Longstreth et al., 1981 Nigam et al., 1984 Prior and Whorwell, 1987 Toskes et al., 1993 Ritchie and Truelove, 1979 Ritchie and Truelove, 1980 Subtotal (95%CI) (41% pla vs 64% treatment) Test for heterogeneity chi square=13.44; P=0.062 Test for overall effect z=6.31; P<0.0001 INSOLUBLE FIBRE Cook et al., 1990 Fowlie et al., 1992 Snook and Shepherd, 1994 Soltoft et al., 1976 Subtotal (95%CI) (56% pla vs 50% treatment) Test for heterogeneity chi square=0.68; P=0.88 Test for overall effect z=-1.01; P=0.3 Total (95%CI) (45% pla vs 60% treatment) Test for heterogeneity chi square=27.97; P=0.0033 Test for overall effect z=4.93; P<0.00001 -1 -2 Favours control Bijkerk et al, Aliment Pharmacol Ther 2004;19:245 1 5 10 Favours treatment 500 g / die 200 g / die + = 25 g. di fibre Long term efficacy of PEG (17.5 gr. bid) vs placebo % pts with normal bowel movements on bowel movement frequency in 70 patients with constipation 90 75 RUN IN PEG PLA 60 * p < 0.001 45 30 15 0 4 8 Corazziari et al, Gut 2000;46:522-6 12 16 20 24 wks Effect of PEG vs. Lactulose on Stool Frequency / Wk PEG better than Lactulose for the following outcomes: - stool frequency / wk - form of stools - relief of abdominal pain - need for additional products Lee-Robichaud et al., Cochrane Database Syst Rev. 2010 Jul 7;(7):CD007570 IBS: profile of an ideal drug • Active in all IBS patients • Efficacy for the multiple aspects of the IBS symptom complex • Devoid of significant side effects • Sustained activity over time • Rapid onset of action • Aimed at underlying pathophysiology • Improves socio-economic impact of IBS IBS: Evolving understanding 5-HT mediated visceral hypersensitivity and gut motility Brain-gut interaction Visceral hypersenstivity Abnormal motor function 1950 1960 Drossman et al, 1999 1970 1980 1990 2000 Distribution of 5-hydroxytryptamine (5-HT) CNS - 5% GI tract - 95% enterochromaffin cells neuronal Gershon, 1999 Serotonin (5-HT): key mediator of gut motility and visceral sensitivity CNS – 5% Activation of 5-HT4 receptors regulates GI function: – increases motility throughout the GI tract (peristalsis) GI tract – 95% – enterochromaffin cells – neuronal Gershon. Aliment Pharmacol Ther 1999;13:15–30 Crowell. Am J Managed Care 2001;7(Suppl):S252–S260 Lacy, Yu. J Clin Gastroenterol 2002;34:27–33 – inhibits visceral sensitivity (pain) – stimulates intestinal secretion Pharmacological Classes of Prokinetics Motilin receptor agonists Erythromycin Mitemcinal Alemcinal Dopamine receptor antagonists Domperidone Metoclopramide Levosulpiride Itopride Cholinesterase inhibitors Pyridostigmine Itopride 5-HT4 agonists Cisapride Tegaserod Renzapride Clebopride Mosapride Prucalopride Velusetrag Naronapride Linaclotide … Prucalopride targets the receptors involved in the underlying impaired motility Selective and specific stimulation of 5-HT4 receptors on intrinsic sensory neurons1,2 Triggers peristaltic reflex and colonic mass movement3 1Briejer & Bosmans. Eur J Pharmacol 2001;423:71 et al. Gastroenterology 1998;115:370 Rectum 3Prins et al. Br J Pharmacol 2000;131:927 4Bouras et al. Gut 1999;44:682 2Grider Prucalopride significantly accelerates overall colonic transit (p<0.05) and proximal colonic emptying t1/2 (p<0.05)4 Three pivotal prucalopride trials: Main inclusion criteria • Adult patients (≥18 years) of either gender • History of chronic constipation, defined as: – ≤2 spontaneous complete bowel movements/week for a minimum of 6 months – ≥1 of the following symptoms for at least a quarter of stools: • Very hard or hard stools • A sensation of incomplete evacuation • Straining during defaecation The 3 studies had identical inclusion criteria and endpoints so the results can be pooled and analysed together 1Camilleri 3Quigley et al. N Engl J Med 2008;358:2344. 2Tack et al. Gut 2009;58:357 et al. Aliment Pharmacol Ther 2008;29:315 Efficacy in chronic constipation: ≥3 SCBM/week (primary endpoint) (SCBM = spontaneous complete bowel movements) 35 30.9 28.4 *** *** % over 12 weeks 30 23.6 24.7 *** *** 25 19.5 ** 20 15 11.3 10 23.9 23.5 ** ** 23.6 *** 12.1 12.0 9.6 5 0 Camilleri11 (n=1924) Tack2 (n=713) (91% F) Placebo Quigley3 (n=641) (87% F) Prucalopride 2 mg Camilleri4 (n=620) (88% F) Prucalopride 4 mg **p≤0.01 vs. placebo ***p≤0.001 vs. placebo 1Camilleri et al. Gastroenterology 2008;134:A548. 2Tack et al. Gut 2009;58:357 3Quigley et al. Aliment Pharmacol Ther 2008;29:315. 4Camilleri et al. N Engl J Med 2008;358:2344 Efficacy in chronic constipation: Increase of ≥1 SCBM/week (secondary endpoint) 60 47.0 43.1 *** *** % over 12 weeks 50 38.1 *** 40 30 44.1 *** 27.5 24.6 47.3 46.6 *** *** 46.6 42.6 *** *** 25.8 20.9 20 10 0 Pooled data1 (n=1924) Placebo INT–62 (n=713) USA–133 (n=641) Prucalopride 2 mg USA–114 (n=620) Prucalopride 4 mg ***p≤0.001 vs. placebo 1Camilleri et al. Gastroenterology 2008;134:A548. 2Tack et al. Gut 2009;58:357 3Quigley et al. Aliment Pharmacol Ther 2008;29:315. 4Camilleri et al. N Engl J Med 2008;358:2344 Efficacy in chronic constipation: Quality of life % subjects with an average increase of ≥1 point on PAC-QOL satisfaction subscale at Week 12 60% 47.1*** 47.8*** 45.8*** 50% 45.6*** 44.0*** 43.3*** 43.5*** 44.4*** 40% 26.0 30% 25.2 22.2 21.8 20% 10% 0% Pooled INT-6 Placebo USA-13 PRU 2mg USA-11 PRU 4mg ***p<0.001 vs. placebo Tack et al. Gut 2009;58:357 Quigley et al. Aliment Pharmacol Ther 2008;29:315. Camilleri et al. N Engl J Med 2008;358:2344 Efficacy in chronic constipation: Onset of response Median time (range) to first “SBCM” (hours:minutes) Placebo (n=645) 26.5 (5–98) Prucalopride 2 mg (n=640) 2.5 (1–13) * Prucalopride 4 mg (n=639) 2 (1–7) * * p < 0.001 prucalopride vs. placebo SBM: spontaneous bowel movement Camilleri et al. Gastroenterology 2008; 134: A548 Pooled data: Response maintained over the 12-week treatment period 50 % over 12 weeks 40 * * * 30 * * * * * * * * 20 10 0 Placebo Prucalopride 2 mg *p<0.001 vs. placebo for both doses of prucalopride Stanghellini et al. Gut 2009 Abstract [2891] Prucalopride 4 mg * Pooled safety and tolerability: Adverse events Most common drug-related adverse events 30 Patients (%) 25 20 15 10 5 0 Placebo (n=661) Prucalopride 2 mg (n=659) Tack et al. Gastroenterology 2008;134:A530 Prucalopride 4 mg (n=657) Summary • Prucalopride has been evaluated extensively (~2700 patients) – Normalisation of bowel function (≥3 SCBM/week) compared with placebo – An improvement in bowel function (≥1 SCBM/week) compared with placebo – Adverse events occurred primarily on Day 1 – No indication of QT prolongation – Efficacy maintained in the long-term • Prucalopride (1‒2 mg) is authorised in Europe for the symptomatic treatment of chronic constipation in women in whom laxatives fail to provide adequate relief • Recommendation by an expert panel is to use this drug when 2 different laxatives have failed to provide relief *P≤ 0.001, vs. PLA **P≤ 0.01, vs. PLA 1276 patients; Linaclotide od for 12 wks Primary endpoint: 3CSBM Lembo et al., N Engl J Med 2011;365:527-36 ERNST E. ABDOMINAL MASSAGE THERAPY FOR CHRONIC CONSTIPATION: A SYSTEMATIC REVIEW OF CONTROLLED CLINICAL TRIALS Forsch. Komplementarmed, 1999
Scaricare