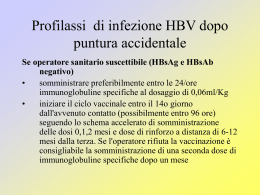
I NUOVI FARMACI PER L' EPATITE C NEI PAZIENTI TALASSEMICI, ONCOEMATOLOGICI ED EMODIALIZZATI Vito Di Marco Gastroenterology & Hepatology Di.Bi.M.I.S. University of Palermo Patients with chronic HCV disease and co-morbidities Key points First point: What is the role of HCV infection in the clinical course of primary disease? Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for patients with HCV chronic hepatitis? • yesterday • today • tomorrow Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow Liver disease in chelated transfusion-dependent thalassemics: the role of iron overload and chronic hepatitis C. V. Di Marco, M. Capra et al. Haematologica, 2008 Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow Baseline features of 376 thalassemia patients according to HCV status in 1993 HCV-RNA negative 189 pts (50.2%) HCV-RNA positive 187pts (49.8%) Age (years, mean, SD) 16 ± 9.3 20 ± 7.1 Gender ( males, %) 89 (47%) 96 (51%) 147 42 67 120 1,501 (288 – 9,720) 1,361 (133 – 8,240) 11 13 14 19 Serum ALT • normal values • upper normal limit Serum Ferritin (ng/mL, median, range) Diabetes Cardiac disease 28 Patients (7%) were drop-out (V. Di Marco, L. Cuccia , A. Maggio, M. Rizzo, C. Gerardi et al, 2014 HCV chronic infection and liver decompensation or HCC p < 0.001 (V. Di Marco, F. Bronte, L. Cuccia , A. Maggio, C. Gerardi et al, 2014 HCV chronic infection and heart failure p = 0.0012 (V. Di Marco, F. Bronte, L. Cuccia , A. Maggio, C. Gerardi et al, 2014 HCV chronic infection and overall survival p < 0.001 (V. Di Marco, F. Bronte, L. Cuccia , A. Maggio, C. Gerardi et al, 2014 Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow Biomarkers, surrogate end-points and true clinical end-points Antiviral Tx Disease Stage HCV-RNA clearance Death Liver Transplant Intermediate end-points 1. Liver Decompensation 2. Heart Decompensation The biomarker is a solid end-point if: 1. It lies in a causal pathway of the disease process 2. It is modified by the intervention, 3. The modification of biomaker influence the clinical course of the disease Alfa 2b-interferon monotherapy in thalassemic patients with chronic C hepatitis. Authors Cuntries N. of patients Mean age Pts with cirrhosis IFN dose Months of therapy Rate of SVR(*) Clemente (1994) Italy 51 14 0% 3 MU/mq t.i.w. 15 37% Di Marco (1997) Italy 70 14 15% 3 MU/mq t.i.w. 12 40% Spiliopoulou (1999) Grecee 13 14 7.5% 3 MU t.i.w. 18 75% Sievert (2002) Australia 28 26 3.5% 3 MU t.i.w. 6 28% (*) SVR: sustained virological response: V. Di Marco et al. Blood, 1997 Viral genotypes and Sustained Virological Response (SVR) to alpha Interferon in Thalassemia Major patients 100 Therapy: alpha IFN 3 MU/mq for 48 weeks SVR 90 80 NR 71.6% 70 (p < 0.001) 60 66.% 50 33.3% 40 30 28.4 % 20 10 0 Genotypes 1 & 4 Genotypes 2 & 3 (n= 109) (n= 30) V. Di Marco et al, Gastroenterology 2007 IL28B status and SVR in 114 thalassemia major patients receiving IFN monotherapy. V. Di Marco et al. Haematologica 2012;97 679-686 Disease events in 141 thalassemics with chronic C hepatitis treated with IFN monotherapy Liver Event Incidence of Liver Disease Complication % 20 55 patients (39%) with Sustained virological Response 86 patients (61%) without Sustained Virological Response 18 16 14 12% 12 Log Rank (Mantel Cox): p = 0.012 SVR 10 0 1 8 6 4 0% 2 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Follow-up (years) Number at risk Group: 0 86 86 Group: 1 55 55 85 85 85 83 82 80 57 52 52 51 49 47 44 42 39 39 55 55 54 53 53 53 53 52 52 52 49 48 48 47 45 45 (V. Di Marco, Z. Borsellino, A. Maggio, C. Gerardi et al,) Survival in 141 thalassemics with chronic C hepatitis treated with IFN monotherapy Mortality 100 98 96 94 92 90 88 86 84 82 80 78 76 96% SVR 0 1 Log Rank (Mantel Cox): p = 0.007 1 2 3 4 5 6 78% 7 8 9 10 11 12 13 14 15 16 17 Follow-up(years) Number at risk Group: 0 86 86 85 85 84 82 57 55 48 46 45 44 41 38 34 31 31 Group: 1 55 55 55 55 55 53 52 52 51 51 51 48 47 46 45 42 42 (V. Di Marco, Z. Borsellino, A. Maggio, C. Gerardi et al,) Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow Baseline features of 230 Thalassemia patients with chronic hepatitis C treated with PEG-IFN and RBV Genotype 1 136 pts (59.1%) Genotype 2 74 pts (32.2%) Genotype 3 8 pts (3.5%) Genotype 4 12 pts (5.2%) Age (years, mean, SD) 36.5 ± 5.9 35.8 ± 6.0 34.9 ± 6.1 32.8± 7.0 Gender ( males, %) 77 (56.6%) 35 (47.3%) 6 (75%) 8 (66.6%) Diagnosis : Chronic Hepatitis Cirrhosis 106 (78%) 30 (22%) 61 (82.4%) 13 (17.6%) 6 (75%) 2 (25%) 10 (83.3%) 2 (16.7%) Serum ALT (IU/L, mean, range) 79 (16 -351) 65 ( 14-750) 114 (30-307) 100 (23-514) Serum Ferritin (ng/mL, mean, range) 919 (19 - 7,000) 1,350,837 (1,28017,700,000) 899 (117-4,470) 1,391,913 (2,2908,193,000) 1225 (200-3471) 808 (260-610) 836,862 (85,034-2,148,00) 785,163 (2908-6,700,000) Serum HCV-RNA levels < 400,000 IU/L > 400,000 IU/mL 64 (39.7%) 72 (60.3%) 28 (37.8%) 46 (62.2%) 3 (37.5%) 5 (62.5%) 7 (70%) 3 (30%) IL 28B (169 patients): CC CT/TT 29 (26.8%) 79 (73.2%) 20 (40%) 30 (60%) 1 (25%) 3 (75%) 4 (50%) 3 (50%) Treatment status: Naive to antiviral treatment Previuos IFN treatment 72 (52.9%) 64 (47.1%) 61 (82.4%) 13 (17.6%) 3 (37.5%) 5 (62.5%) 10 (83.3%) 2 (16.7%) Serum HCV-RNA (IU/L, mean, range) V. Di Marco et al, manuscript in progress Kinetic of virological response according with viral genotypes (Intention to treat analysis) 90% SVR EVR RVR 88% 75% 67% Patients (%) 57% 62% 62% 42% 37% 33% 22% V. Di Marco et al, manuscript in progress Kinetic of virological response in 108 genotype 1 patients (Intention to treat analysis) RVR SVR ETR 90% 81% 81% 72% Patients (%) 66% 55% 49% 43% 38% 23% 14% 11% V. Di Marco et al, manuscript in progress SVR according with viral genotypes and RVR (Intention to treat analysis) RVR NO RVR 86% Patients with SVR (%) 78% 75% 60% 34% 29% 25% 0% n. patients V. Di Marco et al, manuscript in progress Blood transfusion during therapy Increase of blood transfusion during therapy (%) 28% 25% 10% 24 13% 12% 28 66 56 32 12% 24 n. patients V. Di Marco et al, manuscript in progress Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow 12 weeks of Sofosbuvir + Peg-IFN + Ribavirin in naïve patients with chronic HCV hepatitis (genotypes 1 and 4) SVR12 According to Fibrosis Level SVR12 According to Genotype 100 89 96 100 100 SVR12 (%) SVR12 (%) 80 80 80 60 40 20 60 40 20 n/N = 261/292 0 92 GT 1 27/28 GT 4 Lawitz E, et al. N Engl J Med. 2013;369:678-9. 252/273 7/7 GT 5,6 0 No Cirrhosis 43/54 Cirrhosis Sofosbuvir + Ribavirin in patients with chronic HCV hepatitis infected by genotype 2 or 3 Patient Population Genotype 2 Genotype 3 N SVR12 Overall N Cirrhosis SVR12 Cirrhosis Rx Naive 70 97% 11 91% Rx Limited 109 92% 17 94% 12 weeks 36 88% 10 60% 16 weeks 32 94% 9 78% Rx Naive 183 56% 38 34% Rx Limited 98 68% 14 32% 12 weeks 64 30% 26 19% 16 weeks 63 62% 23 61% Treatment Experienced: Treatment Experienced: Sofosbuvir + peg-IFN + Ribavirin for 12 weeks in experienced genotype 2 or genotype 3 patients. Sofosbuvir 400mg + PEG-IFN + ribavirin 1000–1200 mg for 12 weeks, 96 83 100 93 9/9 13/14 83 83 SVR12 (%) SVR12 (%) 89 42/47 26 22/23 20/24 Lawitz E, et al. AASLD 2013, Washington DC. #LB-4 10/12 10/12 No cirrhosis Cirrhosis Indipendent Study: Efficacy and tolerability of Sofosbivir associated with Ribavirin (± Peg-Interferon) in thalassemia patients with chronic hepatitis C Coordinator: Prof. Vito Di Marco, Palermo, Italy Primary Endpoint: The Sustained Virological Response (SVR), defined as the absence of HCV-RNA in serum by a highly sensitive test at the end of treatment and 6 months later. Secondary Endpoints(s): The increase in the number of blood transfusions required to maintain hemoglobin above 9 g/dL during the therapy Group 1: Patients with HCV Genotype 1 infection Duration of therapy: 12 weeks Drugs: Sofosbuvir, 400 mg orally/daily plus Ribavirin, 1000-1200 mg orally/ daily plus alfa-2a Peg-IFN,180 μg subcutaneously/ weekly Group 2: Patients with HCV Genotype 2 Infection Duration of therapy: 12 weeks Drugs: Sofosbuvir, 400 mg orally/ daily plus Ribavirin, 1000-1200 mg orally/ daily Group 3: Patients with HCV Genotype 3 Infection Duration of therapy: 12 weeks Drugs: Sofosbuvir, 400 mg orally/ daily plus Ribavirin, 1000-1200 mg orally/ daily plus alfa-2a Peg-IFN, 180 μg subcutaneously/weekly Group 4: Patients with HCV Genotype 1 or 3 unable to take IFN Duration of therapy: 24 weeks Drugs: Sofosbuvir, 400 mg orally/ daily plus Ribavirin, 1000-1200 mg orally/ daily Centers Center Principal Investigator U.O.C. di Gastroenterologia e Epatologia , Prof Vito Di Marco Azienda Ospedaliera Universitaria “Paolo e-mail: [email protected] Giaccone” Palermo U.O.C. di Gastroenterologia ed Epatologia, Fondazione IRCCS Cà Granda Ospedale Maggiore Milano, Dr.ssa Roberta D’Ambrosio e-mail: [email protected] U.O.C. di Gastroenterologia, Azienda Ospedaliero Universitaria San Luigi Gonzaga, Orbassano, Torino. Prof Giorgio Maria Saracco e-mail: [email protected] U.O.S. "Diagnosi e Terapia delle Epatopatie" e Ambulatorio Trapianto di Fegato, IRCCS Azienda Universitaria Ospedaliera, San Martino-IST, Genova, Prof. Antonino Picciotto e-mail: [email protected] U.O.S.C. di Epatologia, Azienda Ospedaliera di Rilievo Nazionale "A. Cardarelli", Napoli Dr Alfonso Galeota Lanza e-mail: [email protected] Key points First point: What is the role of HCV in the clinical course of Thalassemia Major? • severity of liver disease • complications of disease and survival Second point: What is the benefit of HCV clearance ? (The Sustained Virological Response) Third point: What are the therapeutic options for thalassemia patients with HCV chronic hepatitis? • yesterday • today • tomorrow A Phase III Double Blind Clinical Trial to Study the Efficacy and Safety of the Combination Regimen of MK-5172 and MK-8742 in Treatment-Naïve Subjects with Chronic HCV GT1, GT4, GT5, and GT6 Infection with Inherited Blood Disorders with and without HIV Co-Infection MK-5172 (Gazaprovir): inhibitor of viral protease, NS3/4A, with pangenotypic activity MK-8742 (Elbasvir): inhibitor of HCV non-structural protein, 5A (NS5A) Phase 2 studies: • A total of 899 patients with HCV have received MK-5172 for up to 18 weeks in combinations with PR (PN003 and PN038), in combination with RBV alone (PN039 and PN047), or in combination with MK-8742 +/-RBV (PN035 and PN047). • The patients included were GT 1, 2, 4, 5 or 6, non cirrhotic or cirrhotic, prior PR treatment failures, or HIV co-infected. • The dose range studied has been 25 mg – 800 mg QD. • SVR: > 90% The Study include: HCV Patients with Sickle Cell (SS) Anemia, n=88 HCV Patients with βThalassemia, n=88 HCV Patients with Hemophilia A or B, n=19 Arm 1: Immediate Treatment: Galzaprovir 100 mg plus Elbasvir 50mg for 12 weeks + 24 weeks of follow-up Arm 2: Deferred Treatment: Placebo for 12 weeks + 4 weeks of follow-up, then open label treatment Galzaprovir 100 mg plus Elbasvir 50mg for 12 weeks + 24 weeks of follow-up Hepatitis C-associated B-cell non-Hodgkin lymphomas. B-NHL subtypes most frequently associated with HCV: marginal zone lymphoma diffuse large B-cell lymphoma. Three theories: 1. continuous external stimulation of lymphocyte receptors by viral antigens and consecutive proliferation; 2. HCV replication in B cells with oncogenic effect mediated by intracellular viral proteins; 3. permanent B-cell damage, e.g., mutation of tumor suppressor genes, caused by a transiently intracellular virus (‘‘hit and run’’ theory). J Peveling-Oberhag, Journal Hep 2013; 59:169–177 Chronic HCV infection and lymphoproliferative disorders: mixed cryoglobulinemia syndrome, MGUS and B-cell non-Hodgkin lymphoma G. Caviglia, J Gastroenterol Hepatol. 2014 Oct 28 Chronic HCV infection and lymphoproliferative disorders: mixed cryoglobulinemia syndrome, MGUS and B-cell non-Hodgkin lymphoma Cirrhosis is an additional risk factor for the development of lymphoproliferative disorders in patients with chronic HCV infection. G. Caviglia, J Gastroenterol Hepatol. 2014 Oct 28 Clinical outcome of hepatitis C virus-positive diffuse large Bcell lymphoma patients according to retrospective studies C. Visco World J Gastroenterol 2014 ; 20: 11054-11061 Antiviral therapy is associated with a better survival in patients with hepatitis C virus and B-cell non-Hodgkin lymphomas (ANRS HC-13 lympho-C study) Multicentric study: 116 HCV-positive patients with B-NHL between 2006 and 2012. 45 (39%) marginal zone lymphoma (MZL) 45 (39%) diffuse large B-cell lymphoma (DLBCL) 26 (22%) other types Among 55 patients receiving AT, a SVR was achieved in 23 of 38 (61%) patients with MZL 9 of 17 (53%) with DLBCL . J-M Michot. American Journal of Hematology, 2014 Antiviral therapy is associated with a better survival in patients with hepatitis C virus and B-cell non-Hodgkin lymphomas (ANRS HC-13 lympho-C study) Outcomes of HCV-associated B-NHL according to the cytohistological Groups. J-M Michot. American Journal of Hematology, 2014 Antiviral therapy is associated with a better survival in patients with hepatitis C virus and B-cell non-Hodgkin lymphomas (ANRS HC-13 lympho-C study) Outcomes of HCV-associated B-NHL according to HCV antiviral Treatment. J-M Michot. American Journal of Hematology, 2014 Antiviral treatment in patients with indolent B-cell lymphomas associated with HCV infection: a study of the Fondazione Italiana Linfomi. Cohort study of 704 consecutive HIV-negative, HCV-positive patients with indolent NHL diagnosed and treated from 1993 to 2009 in 39 centers of the Fondazione Italiana Linfomi; 5-year overall survival (OS): 78% [95% CI: 74%-82%] 5-year progression-free survival (PFS): 48% (95% CI: 44%-53%). Multivariate analysis, the use of AT during the patients' life had positive impact on OS. Forty-four of the 100 patients treated with first-line AT achieved a complete remission (CR) and 33 a partial response (PR). HCV-RNA clearance was achieved in 80 patients and was related to lymphoma response. At a median follow-up of 3.6 years, 5-year PFS was 63% (95% CI: 50%-73%). CR + PR rate was 85% with AT as second-line treatment. Arcaini L, Ann Oncol. 2014 Hepatitis C infection is very rarely treated among hemodialysis patients. The Dialysis Outcomes and Practice Patterns Study: • Observational study included 49,762 HD patients in 12 nations (1996-2011). • 4,735 patients (9.5%) were HCV+ • 48 (1.0%) of the 4,589 HCV+ patients with prescription data received antiviral therapy. • 617 HCV+ patients on a waiting list for renal transplantation, only 3.7% were receiving treatment. After restricting to HCV+ patients with overlapping propensity for antiviral treatment, 4 (9.5%) of 42 treated patients and 638 (21.0%) of 3,037 untreated patients died. The hazard ratio for adjusted mortality comparing treated patients with untreated patients was 0.47 (95% CI, 0.17-1.26). Goodkin DA Am J Nephrol. 2013 Antiviral therapy (pegylated interferon and ribavirin) of hepatitis C in dialysis patients: meta-analysis of clinical studies Characteristics of clinical studies: demographic data Characteristics of clinical studies and histologic and virological data F. Fabrizi, Journal of Viral Hepatitis, 2014, 21, 681–689 Antiviral therapy (pegylated interferon and ribavirin) of hepatitis C in dialysis patients: meta-analysis of clinical studies F. Fabrizi, Journal of Viral Hepatitis, 2014, 21, 681–689 J Hepatol. 2013 Treatment of patients with co-morbidities Haemodialysis patients. Treatment of patients with co-morbidities Haemoglobinopathies. Who should be treated: EASL recommendations 2014 In principle, all patients with chronic HCV infection, but in a situation of limited availability: • F3-F4: Priority Patients with NHL Patients on dialysis • F2: Reasonable Thalassemia patients • F0-F1: Debatable Informed deferral of treatment for patients with mild disease EASL Online Recommendations on Treatment of Hepatitis C, April 2014 What about the patient in your clinic today?
Scaricare