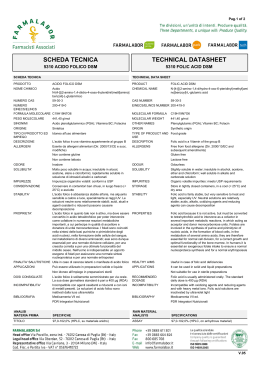
Omocisteina e riproduzione femminile Prof. Irene Cetin Clinica Ostetrica e Ginecologica Università degli Studi di Milano Ospedale Luigi Sacco Omocisteina e Riproduzione Omocisteina: sulfidril-aminoacido essenziale, derivato dalla metionina Alterazioni genetiche Deficit nutrizionali Iperomocistinemia/omocistinuria Alterazione embriogenesi Fattore trombofilico malformazioni aborto distacco di placenta Preeclampsia IUGR Etiology of Neural Tube Defects diabetes mellitus fever hyperhomocysteinemia increased risk of recurrence nutrition folic acid / vit. B12 low socioeconomic status anticonvulsive drugs folic acid antagonists environment preferably girls NTD preferably white race more common in certain families genetic factors FOLATE DEFICIENCY may impede adequate cell turnover during a critical point in the closure of the neural tube Relationship of red cell folate levels to neural tube defect risk JAMA, December 6, 1995 – Vol 274., No.21 Risk of neural tube defects as a function of red cell folate (based upon Daly 1995 and Ernährungssurvey (nutritional survey) 1988 (Thamm 2001)) Red cell folate level nmol/L % of population Risk increase < 340 3% 8 times 340-453 14% 4 times 453-680 48% 3 times 680-906 22% twice >906 13% ---- RBC folate (nmol/L) Red Cell Blood Folate (nmol/L) Data presented as geometric mean (95% CI) 400µg/d folic acid 800µg/d folic acid 906 nmol/L Placebo 0 4 8 12 16 20 24 BERTI C, BIESALSKI HK, GARTNER R, LAPILLONNE A, PIETRZIK K, POSTON L, REDMAN C, KOLETZKO B, CETIN I. Micronutrients in pregnancy: Current knowledge and unresolved questions. Clin Nutr 2011; 30:689-701 Neural tube defects (NTD) • 1991 MRC Vitamin Study Research Group showed the RECOMMENDATION protective effect of folic acid against the recurrence of NTD Folic acid 400 µg/day for primary prevention (4 mg/day for recurrence) • Hyperhomocysteinemia embryonal toxicity by acting at DNAVitamin level, producing hypomethylation or insufficient B12 fosters cell intake of folic acid, synthesis, structural alterations in the genes implicated in and so even though concentrations of folic acid DNA synthesis. are normal, a deficiency of Vitamin B12 could • levels of homocysteine have been detected in the also increase the who riskare of carriers NTD of MTHFR amniotic fluid of patients mutation and concomitant NTD MRC Vitamin Study Research Group 1991;Pitkin 2007 M. De la Calle, Eur J Obst Gynecol and Rep Biol 107 2003; 125–134 Czeizel AE, New Engl J Med 1992;327:1832–5. Brouwer IA. Eur J Obstet Gynecol 2000;92:183–4. Am J Clin Nutr 2000 Other Congenital Defects • Statistically higher levels of homocysteine in the mothers of children with OFC malformations vs controls (Wong, Teratology, 2001) • Mothers of children with heart defects found that 46% had hyperhomocysteinemia vs 14.3% in controls (Wong, Teratology, 2000) • Folate supplementation significantly reduces the incidence of OFC, as well as defects of the heart, pylorus or urinary tract (Hall et al. 1998; van Rooij, 2004) REPRODUCTIVE HEALTH OUTCOMES Pregnant women do not always meet their increased micronutrient requirements Diet = important determinant of pregnancy outcomes and infant health both in short and long-terms: • significant association between inadequate or poor nutrition and high “reproductive” risks • different impacts of the timing of nutritional insults during gestation on both the overall outcome of pregnancy and the nature of adult diseases (i.e. programming the postnatal pathophysiology [Buckley et al. (2005) Cell Tissue Res 322: 73–79]) potential to affect cell numbers or differentiation in the developing embryo Cetin et al, Hum Reprod Update 2010 Iperomocisteinemia e Outcomes riproduttivi Forges Hum Rep 2007 Iperomocisteinemia e Outcomes riproduttivi Boxmeer Hum Rep 2009 High concentrations of folate in monofollicular fluid are associated with an increased chance of achieving biochemical pregnancy. Nutritional phenotype of pregnancy • Dynamic state: adjustments in nutrient metabolism evolve continuously as the mother switches from an anabolic condition during early pregnancy to a catabolic state during late pregnancy • Three compartments model, i.e, mother/placenta/fetus, each of them has different metabolism - fetal growth regulated by the balance between fetal nutrient demand and maternal-placental nutrient supply Cetin et al, Hum Reprod Update 2010 Homocysteine and pregnancy • Normal homocysteine concentration in non-pregnant women: 5.8-12.8 mmol/l • Homocysteine levels decrease during pregnancy. Most studies conclude that values above 10.9 mmol/l are suggestive of hyperhomocysteinemia during pregnancy • Folate requirements: 5- to 10-fold higher than in the non-pregnant condition (Antony 2007) because of rapid fetal growth, placenta development, uterine enlargement and expansion of blood volume (Tamura & Picciano 2006; Kim et al. 2009). Fekete, Maternal and Child Nutrition 2010 Iperomocisteinemia e trombofilia GRAVIDANZA: stato di ipercoagulabilità FATTORI PRO COAGULANTI FATTORI ANTI COAGULANTI TROMBOFILIA tendenza a sviluppare trombosi conseguenti ad alterazioni del sistema coagulativo o fibrinolitico su base ereditaria o acquisita Implantation and placentation - direct contact of fetal with maternal tissues - culminating in the erosion of maternal tissues by fetal cells Deficient remodelling of the spiral arteries ↓ Placental insufficiency Fetal side ↓ Mismatch in the uterine -umbilical exchange surface ↓ IUGR or abortion Maternal side ↓ Increased oxygen levels ↓ dismission of inflammatory molecules, endothelial damage ↓ PREECLAMPSIA Tot 14 492 pregnancies in 5883 women Am J Clin Nutr 2000 The odds ratios (ORs) are presented with adjustment for parity, year of birth, age of mother at birth, and smoking habit Am J Clin Nutr 2000 Repeated spontaneous miscarriages Direct relationship between high levels of homocysteine and alterations in the vascularisation of chorionic villosities, which presented reduced vascular areas, perimeters and diameters (Hum Reprod 2000) IPEROMOCISTEINEMIA MUTAZIONE MTHFR PREECLAMPSIA IPEROMOCISTEINEMIA MUTAZIONE MTHFR Both hyperhomocysteinaemia and homozygosity for the 677C→T mutation in the MTHFR gene seems to lead to an increased risk of pre-eclampsia. Nelen, ClinChemLabMed 2001;39(8):758–763 Mello et al. Hypertension 2005;46:1270-1274 Preeclampsia and Folate Supplementation • A prospective cohort study on 2951 pregnancies aimed at evaluating the relationship between folic acid supplementation and MTHFR genotype with the risk of pre-eclampsia, showed that supplementation of folic acid in a dose of 1.0 mg in the second trimester is associated with reduced risk of pre-eclampsia (Wen et al. 2008) ANAMNESI PRECONCEZIONALE • età adolescenziale, diete particolari, obesità • condizioni di malassorbimento: obesità, celiachia, altre malattie intestinali, chirurgia bariatrica….. • precedenti episodi trombotici • precedenti eventi riproduttivi sfavorevoli (aborti, preeclampsia, distacco di placenta, IUGR) • terapie mediche come antiepilettici Conclusioni • La supplementazione periconcezionale di acido folico e vitamine del gruppo B riduce significativamente il rischio di NTD e malformazioni fetali • Indicato il dosaggio di tHcy nelle donne con mutazione MTHFR. La mutazione non associata ad iperomocisteinemia non sembra influenzare gli outcomes della gravidanza • Nelle donne con iperomocisteinemia è indicata la supplementazione con vitamine del gruppo B (folato, B6, B12) allo scopo di normalizzare i livelli sierici di omocisteina e ridurre i rischi ad essa associati.
Scaricare