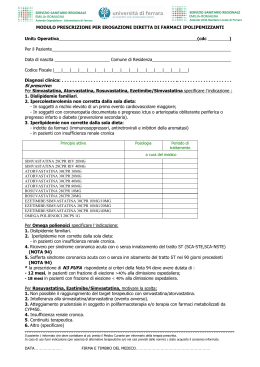
Attualità nell’impiego delle statine Prof. P. Pauletto Dip. di Medicina Clinica e Sperimentale Università degli Studi di Padova U.O. di Medicina Interna I^ U.L.S.S. n° 9, Ospedale di Treviso Risk Factors and Attributable Mortality Reduction — which one stands out as best therapeutic target — Contribution from RF modification • Cholesterol (LDL/HDL) 37% • Blood pressure 14% • Cigarette smoking 6% Contribution comparators • Medical Rx of acute MI 21% • PCI or CABG 16% COLESTEROLO COME FATTORE DI RISCHIO PER LA CARDIOPATIA ISCHEMICA Tassi di mortalità per CHD (%) 35 Stati Uniti RA 200 = 11.5% RA 240 = 13.6% 30 25 RR = 1,18 20 Europa Meridionale RA 200 = 8.5% RA 240 = 10.1% 15 10 RR = 1,18 5 RA = rischio assoluto RR = rischio relativo 0 2.60 (100) 3.25 3.90 4.50 5.15 5.80 6.45 7.10 7.75 8.40 9.05 (125) (150) (175) (200) (225) (250) (275) (300) (325) (350) Colesterolemia totale, mmol/L (mg/dL) Dati dallo studio Seven Countries su 12,467 uomini dell’Europa, USA e Giappone. Verschuren WM et al. JAMA 1995;274:131–136. Correlazione tra CT e mortalità da CHD in uno studio di 25 anni su 12.467 uomini, abitanti in cinque paesi europei, negli USA e in Giappone (da Verschuren et al 1995). Il contributo del FR è lo stesso, ma si parte da livelli basali diversi Le Linee Guida Relationship Between LDL-C Levels and CHD Events — data derived from epidemiologic studies and clinical trials — 3.7 • 2.9 • Relative Risk 2.2 of 1.7 CHD (log scale) • • 1.3 • “Rule of One” applies when LDL < 100 mg/dl 1.0 • 0 40 70 100 130 160 190 220 LDL-Cholesterol (mg/dl) S. Grundy et al. Circulation 2004;110:227-39 HEART PROTECTION STUDY Lancet November 30, 2002, pag 1783 Le Linee Guida: i livelli di LDL-C • NCEP Adult Treatment Panel III update 2004 † National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel, ATP) *TLC: therapeutic lifestyle change (cambiamenti terapeutici dello stile di vita) Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227–239 Rischio alto: CHD o equivalenti del rischio di CHD (rischio di CHD a 10 aa >20%) Obiettivo LDL-C < 100 mg/dl valore ideale opzionale < 70 mg/dl • Joint British Societes 2005 † JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice; Formerly British Heart Journal Journal of the British Cardiac Society Volume 91 Supplement V December 2005 Rischio alto: CHD o equivalenti del rischio di CHD (Total CVD risk† ≥ 20%) Obiettivo LDL-C < 80 mg/dl • European Guidelines On Vascular Disease Prevention in Clinical Practice 2007 Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in ClinicalPractice (Constituted by representatives of nine societies and by invited experts) European Heart Journal (2007) 28, 2375–2414 Rischio alto: CHD o equivalenti del rischio di CHD (rischio di CHD a 10 aa >20%) Obiettivo LDL-C < 100 mg/dl valore auspicabile < 80 mg/dl Le opzioni di trattamento farmacologico Effect of lipid-modifying therapies Therapy Patient tolerability TC LDL HDL TG Bile acid sequestrants Down 20% Down 15–30% Up 3–5% Neutral or up Poor Nicotinic acid Down 25% Down 25% Up 15–30% Down 20–50% Poor to reasonable Fibrates Down 15% Down 5–15% Up 20% Down 20–50% Good Probucol Down 25% Down 10–15% Down 20–30% Neutral Reasonable Down 15–30% Down 24–50% Up 6–12% Down 10-29% Good - Down 18% Up 1% Down 8% Good Statins* Ezetimibe low density lipoprotein, HDLhigh density lipoprotein, TGtriglyceride. TC- total cholesterol, LDLrosuvastatin. *Daily dose of 40mg of each drug. This slide does not include Adapted from Yeshurun D, Gotto AM. Southern Med J1995;88 (4):379-391, KnoppRH. N Engl J Med1999; 341:498 –511, Ezetimibe Prescribing Information. , Estimated change in the five-year relative risk of non-fatal myocardial infarction or CHD death associated with mean LDL-C reduction for the diet, bile-acid sequestrant, surgery, and statin trials (dashed line) along with the 95% probability interval (dotted line). The solid line has a slope=1 J.G. Robinson, J Am Coll Cardiol 2005; 46: 1855-62 CHD EVENTS AND LDL-C IN STATIN TRIALS Lancet 367, 69, 2006 L’ intensità del trattamento con statine e coronaropatia Published at www.nejm.org March 8, 2005 Published at www.nejm.org March 8, 2005 NEJM 350, 2004 Effect of a 3-month lipid lowering therapy on cell composition of carotid plaque C-S AT-10 (ANOVA p=0.031) Percentage of plaque area 24 ┌ - - - 0.017 - - - ┐ ┌ - n.s. - ┐ AT-80 (ANOVA p=0.003) 36 (ANOVA n.s.=0.621) 24 ┌ - - - 0.004 - - - ┐ 32 20 ┌ 0.046 ┐ 20 28 16 ┌ - n.s. - ┐ 24 20 12 16 ┌ - n.s. - ┐ 12 16 8 12 8 8 4 4 4 0 0 Smooth muscle cells 0 Macrophages Lymphocytes P. Pauletto et al, AHA meeting 2009 mg/dL Plasma LDL-Chol levels before and after a 3-month lipid lowering therapy 300 t0 NS 250 NS 200 150 100 50 0 Atorva80 Atorva10 Chol+Sitost t1 Effect of a 3-month lipid lowering therapy on cell composition of carotid plaque 0,140 Cells per area unit Chol+Sitost 0,120 Statin 0,100 0,080 0,060 0,040 0,020 0,000 SMC MO Linpho Il rimodellamento coronarico nei pazienti trattati con statine Intravascular Ultrasound Images at Baseline and Follow-up — an example of plaque regression — Nissen et al. JAMA 2004;291:1079 JAMA 2004;291:1071-1080 JAMA 2006; 295, 13 March JAMA 2006; 295, 13 March Correggendo i livelli di infiammazione si riduce il rischio CV ? CRP in 3745 patients wiht ACS (PROVE IT-TIMI22) Ridker PM et al. NEJM 2005 JUPITER - Primary Endpoint MI, Stroke, UA/Revascularization, CV Death HR 0.56, 95% CI 0.46-0.69 P < 0.00001 0.06 Number Needed to Treat (NNT2) = 95 Number Needed to Treat (NNT5) = 25 * -44% 109 Fewer Events 0.04 *Extrapolated figure based on Altman and Andersen method Rosuvastatin 142 / 8901 0.02 Cumulative Incidence 0.08 Placebo 251 / 8901 0.00 Ridker P et al. N Eng J Med 2008;359: 2195-2207 0 1 2 4 Follow-up (years) Number at Risk Rosuvastatin Placebo 3 8,901 8,901 8,631 8,621 8,412 8,353 6,540 6,508 3,893 3,872 1,958 1,963 1,353 1,333 983 955 544 534 157 174 JUPITER - Primary Endpoint Components Placebo Rosuvastatin n (rate**) n (rate**) [n=8901] [n=8901] HR 95% CI p-value Primary Endpoint 251 (1.36) 142 (0.77) 0.56 0.46-0.69 <0.001* (Time to first occurrence of CV death, MI, stroke, unstable angina, arterial revascularisation) Non-fatal MI Fatal or non-fatal MI 62 (0.33) 68 (0.37) 22 (0.12) 31 (0.17) 0.35 0.46 0.22-0.58 <0.001* 0.30-0.70 0.0002 Non-fatal stroke Fatal or non-fatal stroke 58 (0.31) 64 (0.34) 30 (0.16) 33 (0.18) 0.52 0.52 0.33-0.80 0.34-0.79 Arterial Revascularization 131 (0.71) 71 (0.38) 0.54 0.41-0.72 <0.0001 Unstable angina† 27 (0.14) 16 (0.09) 0.59 0.32-1.10 CV death, stroke, MI 157 (0.85) 83 (0.45) 0.53 0.40-0.69 <0.001* Revascularization or unstable angina 143 (0.77) 76 (0.41) 0.53 0.40-0.70 <0.001* 0.003 0.002 0.09 ** Rates are per 100 person years; † Hospitalisation due to unstable angina; *Actual p-value was < 0.00001 HR – Hazard Ratio; CI – Confidence Limit Ridker P et al. N Eng J Med 2008;359: 2195-2207 0.06 JUPITER - Total Mortality Death from any cause 0.05 -20% 0.02 0.03 0.04 Rosuvastatin 20mg N=198 0.00 0.01 Cumulative Incidence Placebo N=247 Hazard Ratio 0.80 (95% CI 0.67-0.97) p=0.02 0 Number at Risk Rosuvastatin 8,901 Placebo 8,901 1 2 3 4 Follow-up (years) 8,847 8,852 8,787 8,775 6,999 6,987 4,312 4,319 2,268 2,295 1,602 1,614 1,192 1,196 683 684 227 246 Ridker P et al. N Eng J Med 2008;359: 2195-2207 LDL-CT and hs-CRP Levels during the Follow-up Period Baseline level: LDL-CT=108 mg/dL both groups; hs-CRP=4.2 vs 4.3 mg/L in placebo PM Ridker, et al. N Engl J Med 2008;359:2195-207 Cumulative Incidence of Cardiovascular Events According to Study Group PM Ridker, et al. N Engl J Med 2008;359:2195-207 Relationship of the proportional reduction in cardiovascular event rate and mean LDL cholesterol difference between treatment groups in published statin trials PM Ridker, et al. N Engl J Med 2008;359:2195-207 - Online Supplemental Appendix The results of JUPITER and the primary prevention of CHD • Should indications for statin treatment be expanded? • How should measurements of hs-CRP be used? JUPITER: potential limitations / warnings • Hard cardiac events 1.8% (157 of 8901 subjects) in the placebo group vs 0.9% (83 of 8901 subjects) in the rosuvastatin group: 120 participants were treated for 1.9 years to prevent one event. • Significantly higher HbA1levels and incidence of diabetes in the rosuvastatin group (3.0%, vs. 2.4% in the placebo group;P=0.01) • The trial did not compare subjects with and those without hs-CRP measurements • Since statins lower both LDL cholesterol and hs-CRP we cannot determine whether CT, a reduction in inflammation, or a combination of both are responsible for the benefit • Meta-regression is not a reliable technique, and the early termination of the trial owing to the efficacy data probably exaggerated the results to some degree Statine e cardiopatie non ischemiche - 53,6% - 61,3% ENDPOINT PRIMARIO -22% p=0,02 GISSI-HF trial: all-cause death (A) and admission for cardiovascular reasons (B) Terapia di associazione ? Statine + Niacina • Negli USA è entrata in commercio l’associazione Lovastatina 20 mg + niacina a lento rilascio (Advicor*) • Possibili vantaggi: maggiore riduzione del colesterolo e trigliceridi, maggior incremento del colesterolo HDL e maggior riduzione delle LDL piccole e dense • Potenziali rischi: maggior rischio di miopatia e rialzo degli enzimi epatici. Peggioramento del controllo metabolico del diabete o della gotta Brown BG, NEJM 2001 - Wolfe ML, Am J Cardiol 2001 - Bays HE, Am J Cardiol 2003 Strategie di incremento del colesterolo HDL • Storiche – Uso dei fibrati (studio VA-HIT, Helsinki Heart Study) – Uso della niacina (studi CLAS, FATS) • Future – Infusione di Apo A1 Milano (Nissen JAMA 2003) – Inibitori della CETP (Brousseau NEJM 2004) Intervento: misure igienico dietetiche Benefici del decremento ponderale (2- 9 kg) Benefici dell’esercizio fisico moderato (20’- 30’ al dì / a gg alterni) • Riduzione dei fattori di rischio: • Riduzione dei fattori di rischio: – Riduzione p.a.: 5- 20 mm Hg/ 10 kg – Riduzione colesterolo LDL 10- 15% • Riduzione della mortalità totale (16- 65%) (Chaturvedi 1995, Eriksson 1998) – Aumento HDL – Riduzione p.a. – Riduzione insulino- resistenza • Riduzione della patologia coronarica del 35-55% (Manson 1992, Lakka 1994) • Riduzione della mortalità cv (31%) e totale (29%) (Bijnen 1998) Variazione % media dal basale del C-LDL calcolato (settimana 12) Ezetimibe associato con simvastatina: efficacia sul C-LDL Ezetimibe 10 mg + simvastatina 20 mg Simvastatina 20 mg 40 mg –36* –36* 80 mg 0 –10 –20 –30 –40 –44 –44 –50 –60 *p<0.01 terapia di associazione vs. statina da sola Tratto da Davidson MH et al J Am Coll Cardiol 2002;40:2125-2134. Variazione % media dalbasale del C-LDL calcolato (settimana 12) Ezetimibe associato con atorvastatina: efficacia sul C-LDL Ezetimibe 10 mg + atorvastatina 10 mg 10 mg Atorvastatina 20 mg 40 mg 80 mg 0 –10 –20 –30 –37* –42* –40 –50 –45* –53 –60 *p<0,01 terapia di associazione vs. statina da sola Tratto da Ballantyne CM et al Circulation 2003;107:2409-2415. –54 Studio sull’associazione fra ezetimibe e simvastatina: risultati raggruppati sul C-LDL Simvastatina (10–80 mg) (n=263) Ezetimibe + simvastatina (10–80 mg) (n=274) Dosi raggruppate 4,66 mmol/l 4,60 mmol/l C-LDL basale Variazione media del C-LDL calcolato (mmol/l) 0 –0,5 –1,0 –1,5 –1,71 –2,0 –2,38 –2,5 –3,0 *p<0,01 terapia di associazione vs. statina da sola Tratto da Davidson MH et al J Am Coll Cardiol 2002;40:2125-2134. –0,67 mmol/l (–28,2%)* Studio sull’associazione fra ezetimibe e atorvastatina: risultati raggruppati sul C-LDL Atorvastatina (10–80 mg) (n=248) Ezetimibe + atorvastatina (10–80 mg) (n=255) Dosi raggruppate 4,69 mmol/l 4,70 mmol/l C-LDL basale Variazione media del C-LDL calcolato (mmol/l) 0 –0,5 –1,0 –1,5 –2,07 –2,0 –2,5 –2,66 –0,59 mmol/l (–22,2%)* –3,0 *p<0,01 terapia di associazione vs. statina da sola Tratto da Ballantyne CM et al Circulation 2003;107:2409-2415; Ballantyne C et al J Am Coll Cardiol 2002;39(suppl A):227A. Ezetimibe associato con statine dall’inizio: conformità dei risultati degli studi Ezetimibe più statina ha fornito un C-LDL più basso del 18 - 24% C-LDL medio (mmol/l) al termine dello studio rispetto alla statina da sola 3,5 Statina da sola Statina + ezetimibe 3,4 3 2,5 2 3,5 2,9 2,6 24% 18% 2,8 23% 2,0 3,4 21% 2,7 2,2 3 2,5 21% 2,7 2 1,5 1,5 1 1 ,5 ,5 0 0 Atorvastatina Simvastatina Pravastatina 3,4 Lovastatina Studio con statina già iniziata Tratto da Dati di Registrazione, MSP; Davidson MH et al J Am Coll Cardiol 2002;40:2125-2134; Melani L et al Eur Heart J 2003;24:717-728. Statina a dose elevata rispetto ad Ezetimibe associato con statina a dose starter (C-LDL) Atorvastatina 80 mg (n=62) Ezetimibe 10 mg + atorvastatina 10 mg (n=65) Simvastatina 80 mg (n=67) Ezetimibe 10 mg + simvastatina 20 mg (n=67) Pravastatina 40 mg (n=69) Ezetimibe 10 mg + pravastatina 10 mg (n=71) Variazione % media alla settimana 12 0 –10 –20 –31 –30 –40 –50 –44 –54 –34 –44 –53 –60 Tratto dalla Worldwide Product Circular (ezetimibe), MSP; Dati di Registrazione, MSP; Ballantyne CM et al Circulation 2003;107:2409-2415; Davidson MH et al J Am Coll Cardiol 2002;40:2125-2134. Efficacia sui trigliceridi: Ezetimibe associato con statine - risultati raggruppati Atorvastatina (n=248) Variazione % media dei TG dal basale alla settimana 12 0 Ezetimibe Ezetimibe + + Simvastatina atorvastatina simvastatina (n=263) (n=255) (n=274) –5 Ezetimibe + Pravastatina pravastatina (n=205) (n=204) –8 –11 –10 –20 –30 10%** –17 –15 –25 Ezetimibe + Lovastatina lovastatina (n=220) (n=192) 7%** –25* 8%** –18 –24 11%** –22 –33* –35 –40 *Variazione mediana; **p<0,01 ezetimibe + dosi raggruppate delle statine vs. dosi raggruppate delle statine da sole Tratto da Ballantyne CM et al Circulation 2003;107:2409-2415; Davidson MH et al J Am Coll Cardiol 2002;40:21252134; Melani L et al Eur Heart J 2003;24:717-728; Kerzner B et al Am J Cardiol 2003;91:418-424. Variazione % media del C-HDL dal basale alla settimana 12 Efficacia sul C- HDL: Ezetimibe associato con statine – risultati raggruppati 10 2%** 8 1% 7 6 4 9 9 7 7 8 5%* 3%* 4 4 2 0 Atorvastatina Ezetimibe Simvastatina Ezetimibe Pravastatina Ezetimibe Lovastatina Ezetimibe (n=248) (n=263) (n=205) (n=220) + + + + atorvastatina simvastatina pravastatina lovastatina (n=255) (n=274) (n=204) (n=192) *p<0,01 ezetimibe + dosi raggruppate della statina vs. dosi raggruppate della statina da sola; **p=0,03 ezetimibe + dosi raggruppate della statina vs. dosi raggruppate della statina da sola. Tratto da Ballantyne CM et al Circulation 2003;107:2409-2415; Davidson MH et al J Am Coll Cardiol 2002;40:2125-2134; Melani L et al Eur Heart J 2003;24:717-728; Kerzner B et al Am J Cardiol 2003;91:418-424. Residual CVD Risk Niacin and Simvastatin P. Pauletto Medicina Interna I^, Treviso University of Padova - Italy Time to the first primary clinical end point (death from coronary causes, nonfatal MI, stroke, or revascularization) Brown BG et al. N Engl J Med 2001;345:1583 Stenosis (%) and minimal luminal diameter for nine proximal lesions, for all lesions, and for lesions in various categories of base-line severity, according to treatment group. Brown BG et al. N Engl J Med 2001;345:1583 Dose ranges and efficacy of statins, ezetimibe, and bile acid sequestrants Runhua H et al. Endocrinol Metab Clin N Am 2009;38:79 Residual CVD Risk After Statin Therapy Alagona P. Am J Manag Care 2009;15:s65 Low HDL-C Is Associated With High CVD Risk Even If LDL-C Levels Are Well-Controlled (TNT Study) Alagona P. Am J Manag Care 2009;15:s65 Strategies for Reducing CHD Risk Alagona P. Am J Manag Care 2009;15:s65 Efficacy of niacin ER/simvastatin combination therapy: SEACOAST I Alagona P. Am J Manag Care 2009;15:s65 Efficacy of niacin ER/simvastatin combination therapy: SEACOAST II Alagona P. Am J Manag Care 2009;15:s65 Fenofibric Acid and Rosuvastatin Combination Therapy in Patients With Mixed Dyslipidemia Alagona P. Am J Manag Care 2009;15:s65
Scaricare