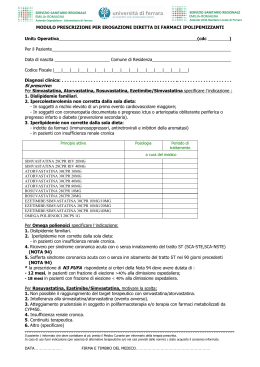
Efficacia e Tollerabilità della Terapia Ipolipemizzante dopo SCA: Ruolo dell’Ezetimibe nei Programmi Integrati di Prevenzione Secondaria Furio Colivicchi Dipartimento Cardiovascolare ACO S.Filippo Neri Roma Relative risk reduction for major coronary events La riduzione del Rischio Relativo risulta indipendente dai livelli iniziali di LDL-C e dalle caratteristiche cliniche del paziente Ogni riduzione di LDL-C di 38 mg/dl si associa ad una riduzione del Rischio Relativo del 24% LDL Cholestrol reduction (mmol/l) Baigent C, et al, Cholesterol Treatment Trialists’ (CTT) Collaborators. Lancet 2005;366:1267–1278. 2011 ESC/EAS Guidelines for the management of Dyslipidaemias: General Indications Every 1.0 mmol/L (38-40 mg/dL) reduction in LDL-C is associated with a corresponding 20-25% reduction in CVD events. An absolute reduction to an LDL-C level <1.8 mmol/L (<70 mg/dL) or at least a 50% relative reduction in LDL-C provides the best benefit in terms of CVD reduction. a: class of recommendation b: level of evidence European Heart Journal 2011;32:1769–1818 Moderate-intensity therapy reduces LDL by 30% to 49% and high-intensity therapy reduces LDL by 50% or more. According to the new guidelines, and considering statin efficacy, only 40 to 80 mg of atorvastatin daily or 20 to 40 mg of rosuvastatin daily may provide such highintensity LDL reduction. Nuova Nota 13 AIFA Nuova Nota 13 AIFA 2011 ESC/EAS Guidelines Meta-analysis on the therapeutic equivalence of statins. European Heart Journal 2011; 323: 1769-1818. Addenda doi:10.1093/eurheartj/ehr169 Risultati Preliminari 3056 pazienti consecutivi con SCA con follow-up di almeno 90 giorni Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):164. Risultati Preliminari 27% dei Pazienti dimessi In terapia con statine 1876 pazienti dose media quotidiana 53 mg 66% dose necessaria a ridurre 50% C-LDL Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):164. Risultati Preliminari Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):164. Risultati Preliminari Il «destino» della terapia ad alto dosaggio con Atorvastatina 80 mg/die a 90 giorni dalla dimissione 779 dimessi con prescrizione di A 80mg/die 398 (51%) continuano Atorvastatina 139 (18%) interrompono il trattamento 80 mg/die 242 (31%) passano ad altra terapia 161 a dose minore di 41 a Atorvastatina Simvastatina 16 ad associazione Eze-Simva 24 a Rosuvastatina Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):164. Sindromi Coronariche Acute Profilo lipidico durante il ricovero ed a 90 giorni dalla dimissione in 3056 pazienti consecutivi con SCA dal Registro Regionale del Lazio Net.Sca 22% con C-LDL≤ 70 mg/dl mg/dl Reported causes of Switch form Intensive Statin Therapy after ACS 1. “Dosage too high” 2. “Afraid of major adverse reactions” Medical Decision 44% Reported Side Effects Dyspepsia Fatigue 56% Side effects Headache Myalgias 0% 20% 40% 60% 80% 100% eGFR < 60 ml/min: HR 1.4 (95% CI, 2.9-1.2) Colivicchi F, et al. Int J Cardiol (2011), 152: 56-60 Asymptomatic increase in liver enzymes Asymptomatic increase in total CK ACC/ AHA Advisory on Safety of Statin Therapy Most adverse events associated with statins appear to occur in patients who are at risk for the condition. For this reason, physicians should be aware of several caveats when prescribing statin therapy. Adverse reactions are more likely to occur at higher statin doses than at lower doses. Consequently, doses should not exceed those required to attain the recommended goal of therapy. As a rule, statin therapy should be employed more cautiously in older persons. Circulation 2002;106:1024-1028. Sindromi Coronariche Acute Funzionalità renale (eGFR stimato con formula MDRD) in 3056 pazienti consecutivi con SCA dal Registro Regionale del Lazio Net.Sca Nuova Nota 13 AIFA Variazione % media dal basale del C-LDL calcolato (settimana 12) Ezetimibe associato con atorvastatina: Risultati dell’efficacia sul C-LDL Ezetimibe 10 mg + atorvastatina 10 mg Atorvastatina 10 mg 20 mg 40 mg 80 mg 0 –10 –20 –30 –37* –42* –40 –50 –53 –60 *p<0,01 terapia di associazione vs. statina da sola Ballantyne CM et al Circulation 2003;107:2409-2415. –45* –54 Intensive LLT in a Comprehensive Secondary Prevention Program 863 ACS patients discharged on atorvastatin 80mg/day* followed for 90 days after discharge 535 (62%) continued atorvastatin 80mg/day 61 (6%) discontinued statin therapy for Major Side effects switched to Ezetimibe 10 mg 277 (32%) with minor side effects or unwilling to continue 113 (13%) switched to a lower dose of atorvastatin 164 (19%) switched to a lower dose of 20-40mg/day 20-40mg/day + Ezetimibe 10 mg atorvastatin *consecutive patients (586 men, mean age 68 ± 13 years) discharged on atorvastatin 80mg/day after an ACS in 2.5 year period Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):136. Intensive LLT in a Comprehensive Secondary Prevention Lipid Profile at 90 days mg/dl * P<0.001 versus A80;. * Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):136. Intensive LLT in a Comprehensive Secondary Prevention Lipid Profile at 90 days Admission Patients LDL-C, mg/dl (mean±SD) Patients with LDL-C <70 mg/dl 124±35 A80 E10 A20-40 A20-40 + E10 535 51 113 164 76±21 104±23 87±31 64±19 213 (39.8%) 6 (11.7%) 27 (23.8%) 108 (65.8%) Colivicchi F, Eur Heart J 2013; 34 (abst.suppl.):136. IMProved Reduction of Outcomes: Vytorin Efficacy International Trial A Multicenter, Double-Blind, Randomized Study to Establish the Clinical Benefit and Safety of Vytorin (Ezetimibe/Simvastatin Tablet) vs Simvastatin Monotherapy in High-Risk Subjects Presenting With Acute Coronary Syndrome Study Design Patients stabilized post ACS ≤ 10 days: LDL-C 50–125*mg/dL (or 50–100**mg/dL if prior lipid-lowering Rx) N=18,144 *3.2mM **2.6mM Standard Medical & Interventional Therapy Simvastatin 40 mg Uptitrated to Simva 80 mg if LDL-C > 79 (adapted per FDA label 2011) Ezetimibe / Simvastatin 10 / 40 mg Follow-up Visit Day 30, every 4 months 90% power to detect ~9% difference Duration: Minimum 2 ½-year follow-up (at least 5250 events) Primary Endpoint: CV death, MI, hospital admission for UA, coronary revascularization (≥ 30 days after randomization), or stroke Cannon CP AHJ 2008;156:826-32; Califf RM NEJM 2009;361:712-7; Blazing MA AHJ 2014;168:205-12 Baseline Characteristics Simvastatin (N=9077) % EZ/Simva (N=9067) % Age (years) 64 64 Female 24 25 Diabetes 27 27 MI prior to index ACS 21 21 STEMI / NSTEMI / UA 29 / 47 / 24 29 / 47 / 24 Days post ACS to rand (IQR) 5 (3, 8) 5 (3, 8) Cath / PCI for ACS event 88 / 70 88 / 70 35 36 95 (79, 110) 95 (79,110) Prior lipid Rx LDL-C at ACS event (mg/dL, IQR) LDL-C and Lipid Changes 1 Yr Mean LDL-C TC TG HDL hsCRP Simva 69.9 145.1 137.1 48.1 3.8 EZ/Simva 53.2 125.8 120.4 48.7 3.3 ∆ in mg/dL -16.7 -19.3 -16.7 +0.6 -0.5 Median Time avg 69.5 vs. 53.7 mg/dL Primary Endpoint — ITT Cardiovascular death, MI, documented unstable angina requiring rehospitalization, coronary revascularization (≥30 days), or stroke HR 0.936 CI (0.887, 0.988) p=0.016 Simva — 34.7% 2742 events NNT= 50 EZ/Simva — 32.7% 2572 events 7-year event rates Individual Cardiovascular Endpoints and CVD/MI/Stroke All-cause death HR 0.99 CVD 1.00 6.8 6.9 0.997 CHD 0.96 5.8 5.7 0.499 MI 0.87 14.8 13.1 0.002 Stroke 0.86 4.8 4.2 0.052 Ischemic stroke 0.79 4.1 3.4 0.008 Cor revasc ≥ 30d 0.95 23.4 21.8 0.107 UA 1.06 1.9 2.1 0.618 CVD/MI/stroke 0.90 22.2 20.4 0.003 0.6 Ezetimibe/Simva Better 1.0 1.4 Simva Better Simva* EZ/Simva* p-value 15.3 15.4 0.782 *7-year event rates (%) Major Pre-specified Subgroups Simva† EZ/Simva† Male Female 34.9 34.0 33.3 31.0 Age < 65 years Age ≥ 65 years 30.8 39.9 29.9 36.4 No diabetes Diabetes 30.8 45.5 30.2 40.0 Prior LLT No prior LLT 43.4 30.0 40.7 28.6 LDL-C > 95 mg/dl LDL-C ≤ 95 mg/dl 31.2 38.4 29.6 36.0 * 0.7 1.0 Ezetimibe/Simva Better 1.3 Simva Better †7-year event rates *p-interaction = 0.023, otherwise > 0.05 Safety — ITT No statistically significant differences in cancer or muscle- or gallbladder-related events Simva n=9077 % EZ/Simva n=9067 % p ALT and/or AST≥3x ULN 2.3 2.5 0.43 Cholecystectomy 1.5 1.5 0.96 Gallbladder-related AEs 3.5 3.1 0.10 Rhabdomyolysis* 0.2 0.1 0.37 Myopathy* 0.1 0.2 0.32 Rhabdo, myopathy, myalgia with CK elevation* 0.6 0.6 0.64 Cancer* (7-yr KM %) 10.2 10.2 0.57 * Adjudicated by Clinical Events Committee % = n/N for the trial duration Relative risk reduction for major coronary events La riduzione del Rischio Relativo risulta indipendente dai livelli iniziali di LDL-C e dalle caratteristiche cliniche del paziente Ogni riduzione di LDL-C di 38 mg/dl si associa ad una riduzione del Rischio Relativo del 24% IMPROVE-IT LDL Cholestrol reduction (mmol/l) Baigent C, et al, Cholesterol Treatment Trialists’ (CTT) Collaborators. Lancet 2005;366:1267–1278. Sindromi Coronariche Acute Intervento farmacologico ipolipemizzante alla dimissione e durante il follow-up – Ruolo dell’Ezetimibe • Ezetimibe è il farmaco di prima scelta in caso di intolleranza assoluta alle statine. • Ezetimibe è utile per favorire il raggiungimento del target lipidico raccomandato. In particolare è consigliabile il suo impiego in associazione a statine ad elevata efficacia nelle seguenti condizioni: 1.Fin dalla dimissione in pazienti con disfunzione renale in associazione a dosi più contenute (20-40 mg) di atorvastatina. 2.Durante il follow-up nei pazienti che non tollerano i dosaggi più elevati di statina
Scaricare