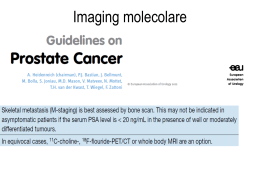
Myocardial Viability and Survival in Ischemic Left Ventricular Dysfunction Robert O. Bonow, MD On behalf of the STICH Trial Investigators Background • LV dysfunction in patients with CAD is not always an irreversible process, as LV function may improve substantially after CABG • Assessment of myocardial viability is often used to predict improvement in LV function after CABG and thus select patients for CABG • Numerous studies have suggested that identification of viable myocardium also predicts improved survival after CABG STICH Viability Hypothesis In this prospective substudy, we tested the hypothesis that assessment of myocardial viability identifies patients with CAD and LV dysfunction who have the greatest survival benefit with CABG compared to aggressive medical therapy STICH Viability Hypothesis • All randomized patients were eligible for viability testing with SPECT myocardial perfusion imaging or dobutamine echo. • Viability testing was optional at enrolling sites and was not a prerequisite for enrollment. Questo è un evidente bias di selezione, e non è stato controllato (forse non è controllabile in un trial di questo genere: è un sottostudio) STICH Viability Hypothesis!!!! SPECT protocols: • Thallium-201 stress-redistribution-reinjection • Thallium-201 rest-redistribution • Nitrate-enhanced Tc-99m perfusion imaging Dobutamine echo protocols: • Staged increase in dobutamine starting at 5 μg/kg/min Quanti hanno fatto il tallio e quanti il tecnezio? Dato mancante. Il tallio stava uscendo dal mercato, arguiamo: pochi pz con tallio? La perfusione con tecneziati sottostima gravemente la vitalità, SPECIALMENTE L’IBERNAZIONE Patients randomized in STICH Revascularization Hypothesis 1212 SPECT n=471 Dobutamine echo n=280 321 150 130 611 Patients with usable myocardial viability test 601 114 487 Viable Nonviable Patients with no usable myocardial viability test Baseline Characteristics Patients With and Without Myocardial Viability Variable Viable (n=487) Non-Viable (n=114) P value Age 61 ± 10 61 ± 9 NS Multivessel CAD 73% 73% NS Proximal LAD stenosis 64% 70% NS Risk score * 12.4 ± 8.7 12.9 ± 9.3 NS Previous MI 76.6% 94.7% <0.001 LV ejection fraction (percent) 28 ± 8 23 ± 9 <0.001 LV end-diastolic volume index (ml/m2) 117 ± 37 147 ± 53 <0.001 LV end-systolic volume index (ml/m2) 86 ± 33 116 ± 50 <0.001 * Significant covariates in risk model: Age, renal function, heart failure, ejection fraction, CAD index, mitral regurgitation, stroke E gli altri 611?????? Myocardial Viability and Mortality Without Viability 1.0 Mortality Rate 0.8 With Viability MED (33 deaths) MED (95 deaths) CABG (25 deaths) CABG (83 deaths) 56% 0.6 35% 0.4 42% 31% 0.2 0.0 0 1 2 3 4 5 Years from Randomization MED 60 51 44 39 29 CABG 54 48 41 41 34 6 0 1 2 3 4 5 Years from Randomization 6 14 4 243 219 206 179 146 94 51 22 12 244 213 203 192 148 94 51 Contraddice tutti gli altri studi, la metanalisi, e non ha senso fisiopatologico. Come è potuto accadere? “Dov’è l’errore?” STICH Viability Hypothesis Limitations: • Lack of viability data in all patients; patients represent a subpopulation of STICH • Analysis limited to SPECT and dobutamine echo, not PET or cardiac MRI Ah, ecco perché! VARIABILITÀ INTERLABORATORIO DELLA VALUTAZIONE DELLA CINETICA REGIONALE DEL VENTRICOLO SINISTRO CON ECO 2D Confronto Esperti vs. Cardiologi liguri Concordanza fra 6 Esperti 51+11% Concordanza fra 44 Cardiologi liguri 41+14% Luigi Badano, 1994 Eco-dobutamina per la vitalità in un grande trial? Senza lettura centrale? Eppure era noto che le ripetibilità dell'esecuzione, della lettura e dell'interpretazione erano scarse e troppo operatore-dipendente per l'ecocardiografia da stress farmacologico… ECO-dobutamina per la vitalità: studi clinici Storia della Medicina: a seguito dell'utilizzo di un test provocativo farmacologico (artefattuale in quanto non fisiologico), nel decorso clinico, a scopo di ricerca, la metodica in studio (ecocardiografia) è stata anche la metodica di riferimento per il giudizio dei risultati ottenuti (miglioramento di cinesi), e nemmeno in condizioni di cecità (in a “publish or perish world”)!! E’ una metodica valida per uno studio multicentrico senza lettura centralizzata? Area di commento libero Ma che STICH e Survey of medical imaging modalities Multimodality imaging devices such as SPECT/CT, PET/CT and PET/MRI encompass the whole spectrum of preclinical and clinical imaging Schober O et al. Eur J Nucl Med Mol Imaging 2009 18-FDG VANTAGGI: - migliore tecnologia PET vs SPET (risoluzione, attenuazione, effetto volume parziale, contrast recovery, migliori aspetti quantitativi) - scarsa dipendenza dal flusso (“tallone d’Achille”della SPET, specie dei tecneziati) Gianni Bisi, 2004 Cardiac Tomography After Nitrate Administration in Patients With Ischemic LV Dysfunction: Relation to Metabolic Imaging by PET Patient 1 Patient 2 He Wei et al. J Nucl Cardiol 2003 Survival by Viability and Treatment 93 Patients with Ischemic Cardiomyopathy and severely depressed left ventricular function Survival Probability With PET Mismatch Without PET Mismatch 1.0 1.0 CABG 0.8 0.6 p = 0.007 Medical 0.4 0.8 CABG 0.6 Medical 0.4 0.2 0.2 NS 0.0 0.0 0 12 24 36 48 Time (months) Di Carli et al, J Thor Cardiovasc Surg 1998; 116: 997 60 0 12 24 36 48 Time (months) 60 Nuclear Imaging Predicts Long-Term Outcome After CABG 100 More Viability Less Viability % Event-free 90 70 p=0.025 50 30 0 12 24 36 Time (Months) From Pagley et al. J Am Coll Cardiol 1996;27:299A. 48 60 Adjusted survival curves for PET and standard arms in Ottawa-FIVE substudy Abraham1 A, J Nucl Med 2010; 51:567–574 FDG IMAGING IN LV ANEURYSMS 70 pts with LV aneurysm 6.8 yrs FU Surgery for viability improved EF and survival (p .0001) Medical therapy with viability had worst outcome (p .0001) Zhang X et al J Nucl Med 2008; 49:1288–1298 STICH Viability Hypothesis Implications: In patients with CAD and LV dysfunction, assessment of myocardial viability does not identify patients who will have the greatest survival benefit from adding CABG to aggressive medical therapy Questo, proprio, no. Tra “viability” e “does” sarebbe stato il caso di aggiungere “, in the way STICH Investigators did,” ma era l’ultima diapositiva, sembrava pedante… Myocardial Viability and Impact of Revascularization Meta-analysis of 24 studies in 3,088 patients Death rate (%/yr) 30 25 -79.6% +23% p < 0.0001 20 16 p = 0.23 Revasc Medical 15 7,7 10 5 6,2 3,2 0 Viable Nonviable Allman et al. J Am Coll Cardiol 2002 “Dopo lo STICH, la vitalità non è più un criterio per l’indica zione a CABG” “Dove stiamo andando ?” Ma che STICH e
Scaricare