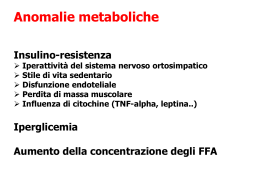
European Heart Journal (1997) 18, 1457-1454 Survey on heart failure in Italian hospital cardiology units Results of the SEOSI study The SEOSI Investigators In 12 days, 3921 patients were enrolled. Mean age was 67 ± 12 years (median 69); 49% of the patients were in NYHA class III-IV; atrial fibrillation was present in 27%; 35% of the cases were scheduled for hospital admission. Ischaemic heart disease was the primary cause of heart failure (42%); arterial hypertension accounted for 20%, idiopathic dilated cardiomyopathy for 15% and cardiac valve disease for 15%. A chest X-ray, ECG and echocardiogram were performed in 70-80% of cases; ambulatory ECG in 36% and exercise testing in 11%. ACE inhibitors were administered to 63-5%, calcium antagonists to 19% and beta-blockers to 5-5%. No significant differences in Introduction Although chronic heart failure is a major and increasingly recognised public health problem, limited epidemiological data are available'1"21'. Recent studies show that treatment of heart failure reduces morbidity and mortality, which nonetheless remain extremely high. Thus, the disease is common, responds to available treatment but has a poor prognosis. A huge economic burden ensues'22'231, hospitalization and instrumental investigation being the major sources of expense. Policies and the attitude of both physicians and patients are the crucial determinants of the overall impact of the disease on the national health system. The Italian Association of Hospital Cardiologist (ANMCO) undertook a nationwide observational study Accepted 14 February 1997. drug prescription were noted in relation to NYHA classification. Multidrug use was common (3-6 ± 1-6). Main advice was: salt restriction (47%) and rest (44%); physical activity and a formal exercise programme were prescribed to 10% and 5% of patients, respectively. Most patients were addressed to hospital follow-up. Thus, heart failure represents a heavy burden for hospital cardiology units. It can be estimated that about 190 000 patients with heart failure seek care at hospital cardiology units each year and about 65 000 are admitted as inpatients. Cardiologists are reasonably well oriented regarding both examinations required and the prescribing of drugs. Beta-blockers and physical exercise are prescribed very cautiously. The format of the present trial, characterized by brevity, simplicity and low cost, could be used as a tool to gain periodical information on several aspects of national health systems and physician behaviour. (Eur Heart J 1997; 18: 1457-1464) Key Words: Heart failure, heart failure units, epidemiology, cardiology hospital care unit, decision making. aimed at assessing the impact of the disease on hospital cardiology units. The hospital was considered as an observatory of a cohort of patients having such symptoms who sought hospital medical care. The main goals of the study were: (1) to evaluate how many patients with suspected or known heart failure consecutively approach a hospital cardiology unit; (2) to assess their clinical characteristics; (3) to define the diagnostic-therapeutic processes set in motion by the cardiologist; (4) to evaluate the social and emotional impact of the disease on the patient. Thus this study was designed to explore one particular area of the cardiological health system rather than be an epidemiological study on heart failure. Methods The ANMCO network has extensive experience in Correspondence: L. Tavazzi, Centro Studi ANMCO, Via La conducting large clinical trials (such as the GISSI studies) and is well trained in pursuing cooperative Marmora 36-50121 Florence, Italy. 0195-668X/97/091457+08 S18.00/0 © 1997 The European Society of Cardiology Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 Three hundred and fifty nine cardiology units participated in a study (SEOSI) coordinated by the Association of Italian Hospital Cardiologists (ANMCO). The aim of the study was to: (1) evaluate how many patients with suspected or known heart failure consecutively approach a hospital cardiology unit; (2) assess their clinical characteristics; (3) define the diagnostic-therapeutic processes set in motion by cardiologists; (4) evaluate the social and emotional impact of the disease on the patient. 1458 SEOSI Investigators investigations. In this favourable setting, a new investigation was set up. The format consisted of a registry with simple forms to be filled in over a short period of time. These were sent to all cardiology units. No grants were offered to the investigators, and cardiologists were invited to participate on the assumption that the study data would lead to a better organized national health system. Out of the 669 hospital cardiology units operating in Italy, 359 centres (54%) participated. Inclusion criteria Data collection and analysis Two questionnaires were to be completed, one by cardiologists, the other by patients. The latter investigated the social and emotional impact of the disease and the patient's satisfaction with the medical care. These results are not reported here. The cardiologist's questionnaire explored the following areas: (1) demography; (2) symptoms and signs of the disease; (3) aetiology; (4) examinations required at the index visit or performed within the previous 3 months; (5) therapy and advice; (6) where the patient was referred to after the index visit. The study forms had to be filled in at enrolment. Thus the examinations listed in the forms were those required by the cardiologist according to his/her intention at the visit. The project was coordinated by ANMCO Research Centre. ANMCO is organised in regional networks; the regional delegates were responsible for the Eur Heart J. Vol. 18, September 1997 Centres Participating Geographical area North Central South Centres' equipment Catheterization laboratory Catheterization laboratory and cardiac surgery None All 41 25 34 37-5 24-5 38 11 9 9 8 80 83 preparation of the study in their areas. The analysis of the data was performed by the Clinical Research Unit of the Salvatore Maugeri Foundation, Gussago, Brescia. A descriptive analysis of data was performed. For comparison of clinical characteristics and treatments a chi-square test was used. Results Over 12 days, 3921 patients were enrolled. Two hundred and nineteen units admitted less than 11 patients; 130 units between 11 and 30, 10 units more than 30 patients. Diagnosis of heart failure was considered by the physician responsible as definite in 84% of the cases, probable in 12%, possible in 3%, and undefined in 1%. It was subsequently confirmed by the coordinating centre, according to the criteria described in the Method section, in 75% of all cases. The main clinical characteristics of the patients are reported in Table 1. Mean heart rate was 85 ± 20 beats . min~'; mean systolic and diastolic blood pressure was 139 ± 25 mmHg and 82 ± 12 mmHg, respectively. Mean age was 67 ±12 years (median 69 years); 25% of patients were aged more than 75 years. The cause of the heart failure was considered certain in 66% of the cases, presumed in 22%, and undefined in 12%. Ischaemic heart disease was the most frequent aetiology (42%: 33% isolated, 9% combined). Seventy percent of these subjects had had a previous myocardial infarction. Hypertensive heart disease was considered to be the primary cause in 15% of the patients (combined in 20%); 35% of these patients at the index visit had a systolic pressure > 160 mmHg, while 30% had a diastolic pressure >95 mmHg. Overall about half of the patients enrolled were in NYHA class III—IV; more than one quarter of the patients had sustained atrial tachyarrhythmias, atrial fibrillation being present in 27-1% of cases, atrial flutter in 11%. Table 2 reports the examinations done within the previous 3 months or required at the index visit. Blood chemistry, ECG, chest X-ray and echocardiogram were performed routinely. Ambulatory ECG was required in Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 The survey lasted 12 days (21 November to 2 December 1994). Over this time, all adult subjects (aged 15 years or more) with proved or suspected heart failure examined either as outpatients or admitted as inpatients to the 359 hospital cardiology units were enrolled. The cardiology units were homogeneously distributed throughout the country. The main cardiological equipment of the participating centres, compared to all Italy's cardiological centres, is reported in Table 1, as a gross indicator of the centres' status. The participating centres are representative of Italy's network of hospital cardiology units. Heart failure was diagnosed as definite, probable, possible or undefined on the bases of the clinical judgement of the physician. No diagnostic criteria were provided, consequently no confirmation of diagnosis was made by the responsible physician. Diagnosis was subsequently checked by the coordinating centre, according to the presence of at least two major criteria or one major and two minor criteria for heart failure in the cardiologists' records. Major criteria were: paroxysmal nocturnal dyspnoea, orthopnoea, pulmonary congestion estimated by physical examination and/or by chest X-ray, presence of third heart sound. Minor criteria were: signs of peripheral congestion (oedema, hepatomegaly, ascites), dyspnoea, <400 m walked without symptoms during normal daily activity. Table I Characteristics of the Italian cardiological centres participating in the study with respect to all national centres Heart failure in Italian CUs Table 2 Demographic and clinical characteristics (n = 3921) 39-6 35-7 24-7 60 4 330 15-3 151 14-7 0-9 0-4 4-9 15-7 76 6-9 43-8 360 12 6 0-7 49-7 331 32-8 75-5 28-2 8-7 0-5 NYHA = New York Heart Association. •"Combined: more than one aetiology primarily involved. Table 3 Examinations required at the index visit or performed within 3 months before enrolment (n = 3921) Electrocardiogram Echocardiogram Chest X-ray Blood chemistry Ambulatory electrocardiogram Exercise test Respiratory function Coronary artery angiography Right heart catheterization Neurohumoral evaluation Myocardial perfusion scintigraphy Radioisotopic ventriculography Cardiac biopsy 814 73-1 690 790 35-8 11-4 7-2 6-5 41 3-6 3-2 2-9 10 35% of the cases, all other examinations much less frequently. Exercise testing was performed in about 11% of patients, in half of them with determination of oxygen consumption. Radioisotopic ventriculography was required in less than 3% of patients. Coronary angiography and perfusional myocardial scintigraphy were mainly required in patients with ischaemic heart disease. Drug treatment according to NYHA class is reported in Table 3; Table 4 gives the medication prescribed according to aetiology. Diuretics were administered to 77% of the patients, ACE inhibitors to 64%, digitalis to 63% and nitrates to 40%. Calcium antagonists were prescribed to 32% of patients with hypertension, 24% of those with ischaemic heart disease, 12% of those with valve disease and 6% of subjects with idiopathic dilated cardiomyopathy. Beta-blockers were administered to 6% and 7% of patients with ischaemic heart disease and idiopathic cardiomyopathy, respectively, and to less than 5% of the other patients, including those with valve disease or hypertension. No significant differences were noted in drug prescription among patients in relation to NYHA classes. The number of drugs prescribed was 36 ± 1-6 and 3-5 ± 1-7 in patients of NYHA classes I and IV, respectively. Therapy was changed at the index visit in 1959 patients; in 72-5% of cases because of symptom deterioration, in 3% because of symptom improvement and in 6% as a result of new information derived from medical literature. In 115 patients, changes in the treatment were due to drug-related adverse effects: calcium antagonists were replaced in 24% of the cases, digitalis in 20%, ACE inhibitors in 19%. Interestingly, 1240 patients (32%) were invited to directly manage the dosage of some drugs, including diuretics (27%) and anticoagulant agents (14%). In 24% of the cases, cardiologists stated that they invited the patients to adjust the dosage of drugs, although they failed to specify which drugs. The advice given by the cardiologists is reported in Table 5. Salt-restriction appears to be frequently recommended to patients of all NYHA classes. Physical exercise was suggested to relatively few patients and a formal programme of physical activity was prescribed to only about 5% of patients (including very light bed exercise inpatients with advanced disease). Twenty-six percent of the patients included were already in hospital at the time of enrolment or admitted immediately after examination as outpatients. A further 7% were listed for eventual hospital admission, and 1-5% were offered evaluation for heart transplantation. Eight percent of the patients were referred to their family physician after the visit and the remaining were invited for subsequent follow-up visits at the hospital cardiology unit. Discussion The SEOSI study evaluated and described the impact of heart failure on Italian hospital cardiology units. It was devised as an investigation of the health system in terms of needs and medical care rather than as an epidemiological study of heart failure. Only those patients presenting themselves spontaneously or referred to hospital cardiology units were considered. Although there are a number of hospital cardiology units throughout the country, a considerable number of patients with heart Eur Heart i, Vol. 18, September 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 Age (years) <65 65-75 >75 Sex Male Aetiology Ischaemic heart disease Idiopathic dilated cardiomyopathy Arterial hypertension Cardiac valve disease Hypertrophic cardiomyopathy Congenital heart disease Others Combined* Symptom duration >2 years NYHA functional Class I Class II Class III Class IV Missing Pulmonary congestion Peripheral congestion Third heart sound <400 m walked without symptoms Tachyarrhythmias Pacemaker Automatic cardioverter-defibrillator 1459 1460 SEOSI Investigators Table 4 Medication (in percent) according to the NYHA classification NYHA class n I 270 II 1718 III 1412 IV 495 All pts 3895* Diuretics ACE inhibitors Digitalis Anticoagulants Antiplatelets Nitrates Calcium antagonists Antiarrhythmics Beta-blockers 58-5 64-8 43-3 151 29-3 30-7 21-5 17-4 12-6 74-4 65-6 59-4 19-8 33-6 35-9 196 180 61 82-6 65-5 70-9 230 30-5 45-8 19 3 19-5 40 79-0 55-2 630 22-6 26-7 39-4 15-8 18-4 3-4 76-8 63-5 62-8 20-9 31 3 396 19-2 18 5 5-5 NYHA = New York Heart Association. *NYHA class evaluation was missing in 26 patients. Table 5 Medication (in percent) according to aetiology Valve disease Idiopathic cardiomyopathy Arterial hypertension 1650 77-6 65-6 56 1 17-2 481 65-3 24-2 20-5 61 891 78-6 51-7 70-8 36-7 19 3 28-4 121 16-2 41 646 86-5 83-6 77-7 25-8 25-1 25-2 6-2 23-4 7-7 840 65-4 57-0 54-0 6-2 21 3 241 31-9 11-2 4-4 T h e total number is greater than 3921 because some patients had more than one aetiology described. failure are managed in other hospital departments, mainly general medicine. These patients were not considered in our study. Furthermore, elementary information, such as diagnosis and aetiology of heart failure, was left to the judgement of individual cardiologists, without restricting predefinitions. Such neutrality, used in other studies'5'91 was intentional, as we aimed at obtaining a realistic picture of the daily impact of heart failure (definite or suspected) on the hospital cardiology units rather than a precise evaluation of the prevalence of the syndrome. The results show that the burden generated by the disease on the health system is remarkable. Assuming that the 310 units not participating in the study show a situation comparable to that of the participating 359 units, (as the type of units and regional distribution would suggest) and that the condition over the short 12 day period can be extended to a year-long term, it can be estimated that in Italy about 190 000 patients with suspected or known heart failure are examined in hospital cardiology units every year. Of these, about 65 000 will probably be admitted to hospital, while about 70% of all patients will have blood examinations, electrocardiograms and echocardiograms. In 1994 the average length of admission for heart failure in Italy was 11 -6 days. From this it follows that heart Eur Heart J, Vol. 18, September 1997 failure accounts for about 777 000 days of cardiological bed occupation per year. A further large number of patients is presumably cared for in general medicine and geriatric units. These rough data illustrate the extent of a public health problem largely unexplored. This becomes critical in our country where until 1994 hospital discharge documents were only used statistically for records. The degree of accuracy (or inaccuracy) in their completion had no implications for either the staff or the hospital of origin, and data were not subjected to any verification. This is particularly worrying for heart failure'24', which is a poorly defined syndrome still difficult to diagnose'25261. In diagnosing heart failure, the cardiologists involved in the SEOSI study had a high degree of accuracy. Central validation of diagnosis was mainly based on clinical evidence of congestion, which in a cardiological setting is probably reasonably specific but, due to the widespread use of diuretics, is not very sensitive. Our criteria for definition of heart failure were similar to those used in the Boston'"'261 and Framingham classification studies'141. They include symptoms and signs associated with severe heart failure, making the recognition of mild or compensated forms of the syndrome difficult. The extent of the public health problem from heart failure emerging from this study is similar to those Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 Patients (n)* Diuretics ACE inhibitors Digitalis Anticoagulants Antiplatelets Nitrates Calcium antagonists Antiarrhythmics Beta-blockers Ischaemic heart disease Heart failure in Italian CUs Table 6 Physician advice (in percent) according to NYHA classification NYHA class Patients (n) I 270 II 1718 III 1412 IV 495 All pts 3895* None Diet limitation Salt restriction Rest prescription Bed rest prescription Physical activity Physical exercise programme Missing 28-5 38-9 370 4-4 3-3 18 9 4-8 2-6 14-6 38-2 47-7 19-7 9-9 151 60 2-6 11-2 331 49-4 30-3 24-8 5-9 4-2 5-2 7-5 28-7 42-6 19-8 600 1-2 1-8 5-4 13 4 351 46-9 22-4 21-2 10-2 4-7 3-9 *NYHA class evaluation was missing in 26 patients. Although different definitions, diagnostic procedures and enrolment criteria in epidemiological studies lead to uneven rates of prevalence and incidence of heart failure, it is clear that both increase markedly with age'10'141. In Northern Italy, in a sample of 6529 subjects, aged 20-64 years, prevalence of heart failure was 6% in people aged 55-59 years and 11-4% in those aged 60-64'131. In 1323 patients consecutively admitted to 26 geriatric wards in Italy in 1992, the prevalence of heart failure was 43-2% in those aged 65-74 years and 58-2% in those >85 years'201. In the U.S.A."41, among the 9405 Framingham Heart Study participants followed for 40 years, the annual incidence of heart failure increased from three cases/1000 in subjects aged 50-59 years to 27 cases/1000 in those aged 80-89. The prevalence also increased from eight cases/1000 subjects aged 50-59 years to 66/1000 in those aged 80-89"41. The mean age of patients enrolled in the SEOSI was 67 years, the median 69, consistent with the observations of the Framingham Heart Study, which reported that heart failure occurs in patients aged 70 years as a mean'141. This aspect, on the mean age of the population, is of great importance since existing clinical trials on drug efficacy in heart failure refer to a decidedly younger population29"321. Enrolment through hospital cardiology units may explain some general features of the study. In the first place, the severity of the disease: about half the patients had moderate to severe heart failure. Presence of atrial fibrillation was frequent, affecting more than one in four patients. Secondly, the aetiology: 42% of patients had ischaemic heart disease, 20% were hypertensive. This latter figure is comparable to that observed in Sweden, but lower than that recognised in the Framingham Study'331. This probably reflects the fact that in Italy patients with ischaemic, valvular or idiopathic heart disease are preferentially referred to hospital cardiology units, while those with hypertension are also referred to general medicine units. A valvular aetiology was more frequent in the SEOSI study than in others'331. Acute rheumatic fever is now uncommon in Italy. Consequences of the disease, however, developing decades later, still exist, especially in the Southern areas. In addition, incidence of degenerative valve diseases is increasing, particularly in the elderly. Thirdly, the instrumental investigation: twodimensional echocardiography is the most frequently used technique in patients with heart failure, confirming that in Italy ventricular function is preferentially assessed by echocardiography. Exercise testing is uncommon and systematically performed only in those hospitals with an interest in heart failure and in patients with severe decompensation. Also, right heart catheterization is routine practice only in patients with severe heart failure, mainly in candidates for heart transplantation. Despite the role of neurohumoral activation in the evolution of the syndrome of heart failure, procedures to assess the neuroendocrine profile of patients are poorly defined and not yet routinely practised in hospital cardiology units. Fourthly, drug treatment: the majority of patients, including those with mild failure, were receiving ACE inhibitors and diuretics. ACE inhibitors are nonetheless still under-used, with a tendency to an even more cautious prescription in severely ill or elderly patients, in whom management of these drugs may be more difficult. On the other hand, prescription of digitalis increased with deterioration of symptoms. Use of nitrates, calcium antagonists and antiarrhythmic agents is influenced more by the aetiology than by the severity of heart failure (i.e. NYHA class). Nitrates are mainly prescribed Eur Heart J, Vol. 18, September 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 in other countries. In the U.S.A., it is estimated that heart failure afflicts more than 3 million people and at least 400 000 new cases of heart failure are diagnosed each year. Despite the advances in therapy, heart failure is the principal cause of death (40 000) and contributes to 250 000 other deaths each year'23-271. In 1991, there were 2 280 445 hospital discharges from non-federal hospitals coded with a primary and secondary diagnosis of heart failure, with an average length of hospitalization of 7-7 days'231. In 1990, 3 458 000 patients with heart failure were seen in an outpatient setting, receiving care over 11 396 000 appointments (3-4 per patient). In 1991, the economic burden of heart failure inpatient care was estimated at 23-1 billion USS. The addition of 270 million USS for heart transplantation in 1800 end-stage patients and the outpatients' costs makes the total health care cost for heart failure in 1991 381 billion USS, that is 5-4% of the total health care expenditure in the U.S.A. that year'231. Similar figures are reported for Europe. In 1989, data from the Swedish National Board of Health and Welfare showed heart failure to be the first-listed diagnosis, accounting for 20% of discharges and more than 30% of days in hospital'221. The total expenditure for heart failure was estimated to be more than 1 million USS (about 800 million SEK for a population of 8 million)'221. The estimated cost of heart failure in the Federal Republic of Germany in 1985 was almost 5 billion USS (6-8 billion DM) for a population of 77 million'91. In the U.K. (with a population of approximately 55 million) 100 000 to 200 000 cases of heart failure are estimated to be admitted annually to hospitals'91. 1461 1462 SEOSI Investigators References [1] Epstein FH, Ostrander LD, Johnson BC et al. Epidemiological studies of cardiovascular disease in a total community — Tecumseh, Michigan. Ann Intern Med 1965; 62: 1170-87. [2] Garrison GE, McDonough JR, Hames CG, Stulb SC. Prevalence of chronic congestive heart failure in the population of Evans County, Georgia. Am J Epidemiol 1966; 83: 338-44. [3] Gibson TC, White KL, Klainer LM. The prevalence of congestive heart failure in two rural communities. J Chron Dis 1966; 19: 141-52. [4] Landhal S, Svanborg A. Astrand K.. Heart volume and the prevalence of certain common cardiovascular disorders at 70 and 75 years of age. Eur Heart J 1984; 5: 326-31. [5] Gillum RF. Heart failure in the United States 1970-1985. Am Heart J 1987: 113: 1043-5. [6] Eriksson H, Svardsudd K. Larsson B et al. Risk factors for heart failure in the general population: the study of men born in 1913. Eur Heart J 1989; 10: 647-56. [7] Brophy JM. Epidemiology of congestive heart failure. Canadian data from 1970 to 1989. Can J Cardiol 1992; 8: 495-8. [8] Phillips SJ, Whinant JP, O'Fallon WM. Frye RL. Prevalence of cardiovascular disease and diabetes mellitus in residents of Rochester, Minnesota. Mayo Clin Proc 1990; 65: 344-59. Eur Heart J, Vol. 18. September 1997 [9] Sutton GC. Epidemiologic aspects of heart failure. Am Heart J 1990; 120: 1538^0. [10] Ghali JK, Cooper R, Ford E. Trends in hospitalization rates for heart failure in the United States, 1973-1986. Evidence for increasing population prevalence. Arch Intern Med 1990; 150: 73-96. [HJShocken DD, Arriet MI, Leaverton PE. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992; 20: 301-6. [12] Remes J, Reunanen A, Aromaa A, Pyorala. Incidence of heart failure in eastern Finland' A population-based surveillance study. Eur Heart J 1992; 13: 588-93. [13] Ambrosio CB, Riva LM, Zamboni S et al. Lo scompenso di cuore nella popolazione: dati di prevalenza. Cardiologia 1992; 37: 685-91. [14] Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 1993; 22(Suppl A): 6A-13A. [15] Rodehefler RI, Jacobsen SJ, Gersh BJ et al. The incidence and prevalence of congestive heart failure in Rochester, Minnesota. Mayo Clin Proc 1993; 68: 1143-50. [16] McMurray J, McDonagh T, Morrison CE. Trends in hospitalization in Scotland 1980-1990. Eur Heart J 1993; 14: 1158-62. [17] Garg R, Packer M, Yusuf S. Heart failure in the 1990s: evaluation of a major public health problem in cardiovascular medicine. J Am Coll Cardiol 1993; 22 (Suppl A): 3A-5A. [18] Andersson B, Waagsteing F. Spectrum and outcome of congestive heart failure in a hospitalized population. Am Heart J 1993; 126: 632-40. [19] Ambrosio GB, Casiglia E, Spolaore P, Vettori P, Baita L, Vescovo C. Prevalence of congestive heart failure (CHF) in elderly. A survey from a population in the Veneto Region Acta Cardiol 1994; 49: 324-7. [20] Rengo F, Acanfora D. Lo scompenso cardiaco nell'anziano. G Ital Cardiol 1994; 24: 1423-34. [21] Sinagra GF, Perkan A, Zecchin M, Camerini F. L'epidemiologia dello scompenso cardiaco: un problema crescente di sanita pubblica. G Ital Cardiol 1995; 25' 1043-53. [22] Eriksson H. Heart failure: a growing public health problem. J Intern Med 1995; 237: 135^1. [23] O'Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. J Heart LungTransp 1993; 13 (Suppl): S107-S112. [24] Romachandran S Vasan, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol 1995; 26: 156574. [25] Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 1991; 12: 315-21. [26] Carlson KJ, Lee DC-S, Goroll AH, Leahy M, Johnson RA. An analysis of physician's reasons for prescribing long-term digitalis therapy in outpatients. J Chron Dis 1985; 38: 733-9. [27] American Heart Association. Heart and stroke facts 1996 Statistical. Supplement in Press. [28] Schocken DD, Arrieta MI, Leaverton PE, Ross EA Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992; 20: 301-6. [29] Cohn JN. Johnson G. Ziesche S et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325' 303-10. [30] Cohn JN, Archibald DG, Ziesche S et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a veterans administrative cooperative study. N Engl J Med 1986; 314: 1547-52. [31] The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left-ventricular ejection fraction and congestive heart failure. N Engl J Med 1991; 325: 293-302. [32] The Captopril-Digoxin Multicenter Research Group. Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. JAMA 1988; 259: 539^4. Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 in patients with ischaemic heart disease. Calcium antagonist administration remains relatively high, probably more than is desirable. Antiarrhythmic drugs are prescribed to about one in five patients, independent of the severity of heart failure. Beta-blockers are almost unused. Multidrug therapy is common. Fifthly, patient care: overall, during the study period, care of most patients was provided by the hospital cardiology units, either as in- or outpatients. Few patients were referred to general practitioners. This is probably peculiar to Italy's health system structure. This information is important at a national level, as it suggests that hospital cardiology units play a major role in the care burden associated with this disease. Sixthly, diffusion of heart transplantation: only a few patients were evaluated for this procedure. This is largely due to the advanced age of the population, but at the same time confirms that in our country transplantation represents a solution for just a minority of patients. Finally, the widespread participation in this study by hospital cardiology units is so encouraging that the same model has been used for other nationwide studies and could perhaps be used elsewhere. The overall cost was only about 30 000 US$. In our view, the brevity, simplicity and low cost of this investigational approach make it a well-suited instrument for responding to public health demands concerning epidemiological evolution, physician behaviour, and the nationwide activities of operative units or laboratories of critical use or high cost. The key point underlining its feasibility is that physicians want to be actively involved in the organization of the new national healthy system, and can do this by providing reliable data. Participation in trials such as SEOSI should be considered part of routine medical activity. Most Italian cardiologists have shown that they agree with this concept. Heart failure in Italian CUs [33] Kannel WB, Ho K, Thorn T. Changing epidemiological features of cardiac failure. Br Heart J 1994; 72 (Suppl): S3-S9. Appendix Participating clinical centres Abbadia S. Salvatore (A. Totteri); Acireale (F. Porto); Acquaviva delle Fonli (G. Grimaldi); Acqui Terme (G. Costantino); Agnone (G. Attademo); Agordo (L. Parissenti); Albano Laziale S. Guiseppe (M. R. Menaguale); Albano Laziale Regina Apostolorum (M. Capo); Albenga (S. Magni); Ancona Umberto I (C. Campodonico); Ancona Sestilli Divisione (L. Quattrini); Ancona Sestilli Servizio (S. Bassotti); Ancona Lancisi II Divisione (G. P. Cesari); Ancona Lancisi Servizio (L. Pasetti); Andria (G. Cannone); Aosta (V. Bigo); Arco (G Mirante Manni); Arezzo (L. Tellini); Ariano Irpino (C. Fiore); Arzignano (M. Boschello); Asti (G. Zola); Augusta (G. Passanisi); Avellino Multizonale Divisione (G. Rosato); Avelhno Multizonale Servizio (M. Genovese); Avezzano (F. Tiburzi); Aviano (G. Calzavara); Badia Polesine (R. Rambaldi); Barga (C. Volterrani); Bari-Carbonara (N. D'Amato); Bari CTO (N. Locuratolo); Bari Mater Dei (M. Tritto); Bari Policlinico Divisione (R. Guglielmi); Bari Policlinico Servizio (M. Campaniello); Bari Policlinico Riabilitazione (G. Castallaneta); Barletta (F. Cappabianca); Battipaglia (M. Maina); Belluno (O. Palatini); Benevento (P. Silvestri); Bergamo (G. Tasca); Bibbiena (M. Marri); Biella (D. Torta); Bisaccia (G. Macina); Bologna Bellaria (G. Di Pasquale); Bologna Maggiore (G. Leonardi); Bologna Malpighi (A. Mirri); Bologna S Orsola (A. Marchesini); Borgomanero (M. Zanetta); Borgosesia (P. Devecchi); Bosisio Parini (G. Gullace); Bovolone (G. Montresor); Brescia (P Faggiano); Brindisi (M. De Giorgi); Cagliari Binaghi (G. Ghia); Cagliari Brotzu (M. Porcu); Cagliari SS Trinita (S. Piras); Caltagirone (S. Cusumano); Camogli (C. Marsano); Campi Salentina (V. Greco); Campoli del Monte Taburno (L. Odierna); Camposampiero (F. Contessotto); Canicatti (G. Marrone); Casarano (A. Marzo); Caserta Divisione (O. Di Maggio); Caserta Servizio (S. Romano); Caserta Prevenzione e Riabilitazione (B. Castellano); Casoli (D. Rotondo); Cassano D'Adda (G. Gibelli); Cassano delle Murge (R. Lagioia); Castel San Giovanni (M. Piepoli); Caslellammare Di Stabia (R. Padricelli); Castelnuovo Garfagnana (P. R. Mariani); Castelnuovo Ne'Monti (U. Guiducci); Castrovillari (F. Dulcetti); Catania S. Curro S Luigi (F. Platania); Catania Cannizzaro Divisione (R. Coco); Catania Cannizzaro Servizio (F. Raimondi); Catania Ferrarotto (V. Calvi); Catania Garibaldi (R. Cardillo); Catania Ascoli Tomaselli (F. Torcitto); Catanzaro Policlinico (M. Affinita); Ceccano (M. Iorio); Cecina (F. Mazzinghi); Cento (N. Paparella); Cerreto Sannita (G. Malgeri); Cesena (C. Garaffoni); Chiaravalle Centrale (A. Raffaele); Chiari (G. Beghelli); Chien (E. Costantini); Cinisello Balsamo (A. Lippolis); Citla di Castello (G. Arcuri); Codogno (C. Guasconi); Colleferro (E. Venturini); Comacchio (P. Yiannacopulu); Como Valduce (G. Tadeo); Como Sant'Anna (A. Politi); Conegliano Venelo (F. Accorsi); Conversano (L. Martino); Correggio (L. Lusetti); Cortona (G. Mannini); Cosenza INRCA (R. Gallo); Cosenza DellAnnunziata (R. M. Manfredi); Cremona (C. Bianchi); Cuasso al Monte (G. Lepori); Cuneo (U. Milanese); Domodossola (G. Sauro); ££o/z (L. Faenza); Empoli (A. Taiti); £rtar (D. Agnelli); Fabriano (P Domenella); Faenza (L.Pirazzini); Fano (P. Rotatori); Fasano del Garda (C. Marchesi); Ferentmo (V. Bernardi); Fermo (P. Paoloni); Ferrara (P. Gruppillo); Fidenza (S. Cantoni); Firenze S. Giovanni (S. Badolati); Firenze Careggi Divisione (R Valenti); Firenze Careggi Servizio (M. Ciacchen); Firenze S. M Nuova (G. Zambaldi); Firenze Camerata (M. Toso); Foligno (F. Patriarchi); /br/i Morgagni-Pierantoni Divisione (G. L. Morgagni); For/i Morgagni-Pierantoni Servizio (M. Milandri); Formia (E. Batosi); Fossombrone (G. Possanzini); Francavilla Fontana (G. Vecchio); Frascati (M. Topai); Frosinone (M. Savona); Fucecchio (A. Geri Brandinelli); Gagliano del Capo (G. Pisa); Gallipoli (F. Mariello); Gavardo (A. Novali); Gemona del Friuli (E. Spinelli); Genova DIMI (G. Molinari); Genova S. Martino I Divisione (P. Rossi); Genova S. Martino II Divisione (S. Mazzantini); Genova S Martino Servizio (D. Papagna); Genova Galliera (F. Chiarelli); Genova Nervi (L. Carratino); Genova Sampierdarena (P. G. Abrile); Genova Sestri Ponente (G. Terzi); Genova Voltri (A. Torriglia); Genzano (F. Gabbarini); Gerace (E. Sirleo); Gorizia (R. Marini); Gravedona (M. R. De Iaco); Grosseto (G. Miracapillo); Grollaglie (R. Ruta); Guastalla (E. lori); Gubbio (S. Sisani); Gussago (M. Volterrani); Imola (S. Negroni); Imperia (S. Acquarone); hernia (G. Evangelista); /vrea (G. Bergandi); L'Aquila (A. Scimia); Lagonegro (V. Viggiano); Lamezia Terme (C. Asciotti); Lanciano (T. Diodato); Larino (G. Laquaglia); Lavagna (P. Rosselli); Z-ecce (M. R. Greco); Legnago (M. Gemelli); Z-eo«/orre (L. Vicari); Livorno (M. Formichi); Locn (G. Martelli); /.orfi (C. Panciroli); Lugo (S. Delia Casa); Magenta (G. Bardelli); Manfredonia (G. Prencipe); Mantova (A. Reggiani); Marino (G. Sarli); Marsala (C. Attardo); Massa (A. Mariani); Massa Marittima (M. Maestrini); Matera (L. Veglia); Mazara del Vallo (I. Fiore); Mercalo San Severino (V. Capuano); Mesagne (V. Santoro); Messina Papardo (A. Coglitore); Messina Piemonte (G. Di Tano); Messina Regina Margherita (P. Iannello); Messina Policlinico (F. Luzza); Meslre (G. Zuin); Milano Monzino (M. Guazzi); Milano Istituto Nazionale Tumori (C. Materazzo); Milano Buzzi (A. Pini); Milano FBF (F. Turazza); Milano Niguarda I Divisione (E. Gronda); Milano Niguarda II Divisione (F. Recalcati); Milano Mellom (M. Picca); Milazzo (C. Coppolino); Mirandola (V. Malavasi); Modena (C. Cappelli); Monfalcone (E. Barducci); Montebelluna (M. Baldo); Montescano (C. Opasich); Monza (F. Valagussa); Morbegno (M. G. Songini); Mozzo (C. Malinverni); yva/>o// C r O (V. Scotto Di Uccio); Napoli Fondazione Pascale (U. Bianchi); Napoli Elena D'Aosta (A. Setaro); Napoli Nuovo Dei Pellegrini (P. Capogrosso); Napoli S. Gennaro (A. Somelli); Napoli Monaldi Divisione (F. D'Isa); Napoli Monaldi Riabilitazione Eur Heart J, Vol. 18, September 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 Steering Committee: L. Tavazzi (Chairman), F. De Giuli, R. Ferrari, A. Maggioni, C. Opasich. Scientific Committee: A. Boccanelli, A. Gavazzi, E. Gronda, C. Opasich, C. Rapezzi, M. Scherillo, G. Sinagra. Writing Committee: L. Tavazzi, R. Ferrari, C. Opasich. Organizing Secretariat: M. Gorini, D. Lucci. ANMCO Regional Delegates: G. Baduini, G. Borrello, D. Bracchetti, E. Braito, A. Circo, C. De Luca, I. De Luca, A. Dessi, F. Furlanello, E. Gatto, M. Giasi, T. Lanzetta, A. Lopizzo, E. Musacchio, A. Notaristefano, P. Pellegrini, E. Petz, G. Saccomanno, A. Santoboni, F. Valagussa. The study was endorsed by the National Association of Hospital Cardiologists. The SEOSI was helped by grants from Schering-Plough and Sigma-Tau, neither were involved in analysis or writing. 1463 1464 SEOSI Investigators Eur Heart J, Vol. 18, September 1997 Policlinico Umberto I Divisione I (B. Fedele); Roma Policlinico Umberto I Divisione II (M. Schiariti); Rossano (S. Salituri); Rovereto (P. Bonmassari); Sacile (M. Valente); San Benedetto del Tronlo (G. Sonaglioni); San Gavino Monreale (G. Giardina); San Giovanni Rotondo (G. P. Perna); San Giovanni Valdarno (G. Mantini); San Pietro Vernotico (S. Pede); San Vito al Tagliamento (M. Duchi); Sanremo (G. C. Benza); Sansepolcro (P. Rossi); Saronno (D. Nassiacos); Sarteano (S. Del Vecchio); Sarzana (D. Bertoli); Sassari (L. Sannia); Sassuolo (P. Bellesi); Savona (A. Gandolfo); Scandiano (G. P. Gambarati); Sciacca (P. Gambino); Sci7/a (M. Musolino); Scorrano (O. De Donno); Semgallia (R. Amici); Seriate (T. Nicoli); Siderno (M. Iannopollo); S/e«a (R. Favilli); Sondalo (F. Fedeli); Sondrio (M. Marieni); Sora (G. Lilla Delia Monica); Soveria Mannelli (A. Marotta); Spoleto (A. Pagano); Sulmona (E. Conti); Teramo (P. Desiati); Terlizzi (F. Troso); Termoli (A. Montano); 7e#-ni (D. Bovelli); Terracina (A. De Angelis); 7%/ene (L. Bassan); rA/eji (G. Poddighe); Torino Giovanni Bosco (M. G. Sclavo); Torino Maria Vittoria (S. Sgambetterra); Tradale Fondazione S. Maugen (R. Bonelli); Tradate Circolo Galmarini (M. Barenghi); Trapani (G. Ledda); Trebisacce (P. Aragona); Trento (G. Mosna); Treviglio (R. Achieri); Treviso (G. Renosto); Tricase (R. Mangia); Trieste Maggiore Divisione (A. Di Lenarda); Trieste Maggiore Servizio (F. Humar); Trieste Maggiore Riabililazione (P. Gori); Troina (A. Puzzo); Udine 1st Medicina Fisica (G. Molinis); Udine S M della Misericordia (M. C. Albanese); Urbino (G. Gheller); Valeggio sul Mincio (G. Perini); Ka//o aW/a Lucania (G. Liguon); Kare.se Z)e/ Po«(e (I. Ghezzi); Varese Di Circolo (F. Morandi); Porto (G. Levantesi); Venezia (S. Valente); Venosa (I. De Tommaso); Verbania (P. Corsetti); Vercelli (J. Makmur); Verona Borgo Trento (R. Rossi); Verona Borgo Trento Riabilitazwne (A. Vicentini); Verona Borgo Roma (P. Benussi); Veruno (F. De Vito); Viareggio (A. Pesola); Vigevano (C. Mazzini); Vimercate (G. Gentile); Viterbo (D. Pontillo); Voghera (M. G. Bergognoni); Ko/ta Mantovana (F. Mascaro); Volterra (L. Francardelli). Downloaded from http://eurheartj.oxfordjournals.org/ by guest on February 10, 2016 (P. Sensale) Nardo (M. C. Carmillo); Negrar (H. Guilarte); Novara (P. Dellavesa); Nuoro (L. Dettori); Olbia (A. Mauric); Oliveto Citra (P. Bottiglieri); Orbassano (R. Pozzi); Oristano (M. Cossu); Ortona (M. Manetta); ftst/a Lido (R. Neri); Padova Divisione (G. M. Boffa); Padova Servizio (G. Bozza); Palermo Buccheri La Ferla FBF (A. Castello); Palermo Civico e Benfratelli (C. Caruso); Palermo Albanese (D. Di Vincenzo); Palermo Ingrassia (F. Clemenza); Palermo Cervello (B. Di Maria); Palermo Policlinico (M. Traina); Palermo Villa Sofia Divisione (A. Leto); Palermo Villa Sofia Servizio (G. Di Piazza); Palmanova (F. G. Pidutti); Paola (M. Balsano); Passirana-Rho (M. Palvarini); Pavj'a (S. Lucreziotti); />en/ie (A. Vacri); Perugia Silvestrini (G. Prodani); Perugia Monteluce (M. Bentivoglio); Pesaro (G. Tarsi); Pescia (G. Chiriatti); Piacenza (D. Gandolfini); Piazza Armerina (M. Farruggio); Piedimonte Matese (F. Vitale); Pietra Ligure (C. Mattiauda); Pinerolo (L. Riva); /Via S. Chiara Divisione (E. Puccini); Pua S1. Chiara Divisione-CNR (C. Carpeggiani); Pua S. Chiara Servizio (M. Ravani); Pistoia (A. Alfleri); Poggio Rusco (M. Negrelli); Policoro (E. De Nittis); Polistena (F. Catananti); /"o//a (F. Turturiello); Pontedera (D. Levantesi); Pordenone (E. Viel); Ponoferraio (A. Davini); Potenza S. Carlo Divisione (M. T. Stigliani); Potenza S. Carlo Servizio (A. Zarrillo); Prata (G. Lauri); Ragusa (V. Spadola); Rapallo (G. Gigli); Ravenna (M. Piancastelli); Reggio Calabria Morelli (E. Tripodi); Reggio Calabria MelacrinoBianchi (G. Neri); Reggio Emilia (F. Burani); R/io (R. Fornerone); Riccione (P. Del Corso); R/e« (A. Mene); Rimini (M. Marzaloni); Rogliano (A. Provenzano); /ioma CTO (G. Gattini); taa INRCA (D. Del Sindaco); Roma to dell'Immacolata (G. L. Biava); Soma Forlanmi (G Cacciatore); Roma 7-W (G. Speciale); Roma 5. Camillo I Divisione (C. Greco); Roma 5. Camillo II Divisione (A. Lacche); Roma 5. Camillo UTIC (M. Carelli); Roma S. Camillo Servizio (L. Boccardi); Roma S. Camillo Poligrafia (G. Minardi); Roma S. Filippo Neri (G. Ansalone); Roma S. Giovanni (G. Scaffidi); Roma S. Pietro FBF (S. Capurso); Roma S. Eugenio (G. Barbato); Roma Policlinico Casilino (A. Pappalardo); Roma
Scarica