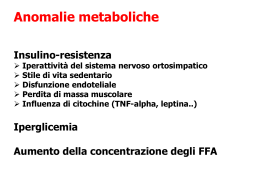
European Heart Journal (2002) 23, 1692–1698 doi:10.1053/euhj.2001.3157, available online at http://www.idealibrary.com on Cumulative effect of complete left bundle-branch block and chronic atrial fibrillation on 1-year mortality and hospitalization in patients with congestive heart failure A report from the Italian network on congestive heart failure (in-CHF database) S. Baldasseroni1, L. De Biase2, C. Fresco3, N. Marchionni4, M. Marini1, G. Masotti4, G. Orsini1, M. Porcu5, F. Pozzar6, M. Scherillo7 and A. P. Maggioni1 on behalf of the Italian Network on Congestive Heart Failure (IN-CHF) Investigators 1 Italian Association of Hospital Cardiologists (ANMCO) Research Center, Florence, Italy; 2S. Andrea Hospital, Department of Cardiology, Rome, Italy; 3S.M. Misericordia Hospital, Department of Cardiology, Udine, Italy; 4 Department of Critical Care Medicine and Surgery, Section of Gerontology and Geriatric Medicine, University of Florence, Azienda Ospedaliera Gareggi, Florence, Italy; 5S. Michele Brotzu Hospital, Department of Cardiology, Cagliari, Italy; 6S. Camillo Hospital, Department of Cardiology, Rome, Italy; 7Monaldi Hospital, Department of Cardiology, Naples, Italy Background Many clinical variables have been proposed as prognostic factors in patients with congestive heart failure. Among these, complete left bundle-branch block and atrial fibrillation are known to impair significantly left ventricular performance in patients with congestive heart failure. However, their combined effect on mortality has been poorly investigated. The aim of this study was to determine whether left bundle-branch block associated with atrial fibrillation had an independent, cumulative effect on mortality for congestive heart failure. Methods and Results We analysed the Italian Network on congestive heart failure (IN-CHF) Registry that was established by the Italian Association of Hospital Cardiologists in 1995. One-year follow-up data were available for 5517 patients. Complete left bundle-branch block and atrial fibrillation were associated in 185 (3·3%) patients. In this population the cause of congestive heart failure was dilated cardiomyopathy (38·4%), ischaemic heart disease (35·1%), hypertensive heart disease (17·3%), and other aetiologies (9·2%). This combination of electrical defects was associated with an increased 1-year mortality from any cause (hazard ratio, HR: 1·88; 95% CI 1·37–2·57) and sudden death (HR: 1·89; 95% CI 1·17–3·03) and 1-year hospitalization rate (HR: 1·83; 95% CI 1·26–2·67). Conclusions In patients with congestive heart failure, the contemporary presence of left bundle-branch block and atrial fibrillation was associated with a significant increase in mortality. This synergistic effect remained significant after adjusting for clinical variables usually associated with advanced heart failure. We can conclude that this combination of electrical disturbances identifies a congestive heart failure specific population with a high risk of mortality. (Eur Heart J, 2002; 23: 1692–1698, doi:10.1053/euhj.2001. 3157) 2002 The European Society of Cardiology. Published by Elsevier Science Ltd. All rights reserved. Key Words: Congestive heart failure, atrial fibrillation, complete left bundle branch-block, prognosis Revision submitted 19 December 2001, and accepted 19 December 2001. The IN-CHF Registry was supported in part by Merck Sharp & Dohme Italy. See the Appendix for a complete list of participating centres and Investigators. Correspondence: Aldo P. Maggioni, MD, ANMCO Research Center, Via La Marmora 34, 50121 Florence, Italy. 0195-668X/02/$35.00 2002 The European Society of Cardiology. Published by Elsevier Science Ltd. All rights reserved. Left bundle-branch block associated with atrial fibrillation in CHF patients Introduction In the last few years, total mortality from heart disease has been declining in industrialized countries as a consequence of improved treatment and primary prevention[1], but the number of patients affected by congestive heart failure is still increasing[1]. This is caused by increasing life-expectancy and the age-associated prevalence of heart diseases in general, and of congestive heart failure in particular[2–4]. Several clinical and pathophysiological factors have been proposed as independent prognostic indicators in patients with congestive heart failure[5–9]. Recently, data concerning the prognostic significance of intraventricular conduction defects and, in particular, of complete left bundle-branch block in congestive heart failure, have also been evaluated[10]. The role of atrial fibrillation in heart failure is still debated. Indeed while there is a strong consensus about the dramatic effect of atrial fibrillation on the haemodynamic profile of patients affected by heart failure[11], its prognostic effect is still under discussion. Data on the prognostic value of atrial fibrillation in congestive heart failure are somewhat conflicting[12,13]. Therefore, we analysed the IN-CHF database on unselected outpatients with congestive heart failure of different aetiologies, followed-up for 1 year by a large number of cardiology centres in Italy, with the purpose of evaluating the prevalence of the association of left bundle-branch block with atrial fibrillation and testing whether this association is characterized by higher mortality and hospitalization rates independently of all other variables. 1693 cardiologist at each participating centre, using a standardized format outlined in the database. This information was used by the computer programme to control for the acceptability of the diagnosis of left bundlebranch block, and to distinguish between incomplete (QRS duration 100–120 ms) and complete (QRS duration d120 ms) associated with morphological criteria block. Patients were followed-up according to the routine clinical practice of the participating centres. In this context, patients underwent standard chest X-ray, 24-h Holter ECG monitoring to confirm the presence of chronic atrial fibrillation, two-dimensional echocardiography, and blood sampling for the most common laboratory tests (e.g. creatinine, electrolytes, etc.), when the attending cardiologists deemed them necessary. Cardiologists at the participating centres were responsible for confirming the contemporary presence of complete left bundle-branch block and atrial fibrillation, for defining the aetiology of congestive heart failure and the NYHA class, reporting that the third heart sound was audible, and computing the cardiothoracic ratio. The left ventricular ejection fraction was calculated from the fourchamber apical echocardiographic view. Ventricular tachycardia was defined as an episode of tachycardia with a widened QRS that lasted longer than three beats, with a heart rate >100 beats . min 1, as revealed by 24-h Holter ECG monitoring. Renal dysfunction was defined as a serum creatinine >2·5 mg . dl 1. Previous hospitalizations for congestive heart failure in the year before entry were also recorded. After the baseline visit, patients were followed-up for at least 1-year. In cases of out-of-hospital death, the event was confirmed by telephone interview with the patient’s relatives, using a standard questionnaire aimed at determining the mode of death (sudden vs non-sudden). Methods Study design, collected data and definitions Data for the present analysis originated from the database of the IN-CHF Registry[14], a survey designed by an ad-hoc Committee of the Italian Association of Hospital Cardiologists (ANMCO, Florence, Italy) in 1995. Onehundred and fifty cardiology centres agreed to participate in the study. While the centres were distributed across the whole country, they were more frequently located in northern (46%) than in central (24%) or southern (30%) Italy, representing the spread of cardiology centres in Italy. Training sessions were organized to prepare clinicians to collect and enter data using an ad-hoc designed software. Patients’ data were recorded at each centre by trained cardiologists and were then pooled into a single database at the ANMCO Research Center. Entry into the database required that patients had a diagnosis of congestive heart failure based on the ESC guidelines[15]. Demographic, clinical, instrumental and laboratory variables, and information on drug therapy were collected for each patient. At baseline, a 12-lead ECG was recorded and coded by a single Study population Between March 1995 and January 2000 a total of 6284 consecutive patients with congestive heart failure completed the 1-year follow-up. Of these 767 (706 affected by congestive heart failure due to primary valvular heart disease and 61 patients underwent heart transplantation) were excluded from the present analysis which includes therefore 5517 patients. Statistical analysis Data were analysed using the SAS statistical package. Continuous variables are presented as meanstandard deviation. The chi-square test was used to test the association of complete left bundle-branch block/atrial fibrillation with several baseline characteristics and 1-year total mortality. Cox proportional hazards multivariate models with calculation of the adjusted hazard ratio and 95% confidence intervals (95% CI) were used to identify the independent determinants of all-cause Eur Heart J, Vol. 23, issue 21, November 2002 1694 S. Baldasseroni et al. Table 1 Demographic and clinical characteristics of the four groups of patients according to the presence of left bundle-branch block (LBBB) or atrial fibrillation (AF) or both: absence of left bundle-branch block and atrial fibrillation (group A) presence of complete left bundle-branch block (group B), presence of atrial fibrillation (group C), presence of atrial fibrillation and complete left bundle-branch block (group D) A B C D (no AF, no LBBB) (no AF, LBBB) (AF, no LBBB) (AF and LBBB) P value (%) (%) (%) (%) Sex (male) Age >70 years NYHA III–IV Ischaemic heart disease Previous hospitalization for chronic heart failure Third heart sound Ejection fraction <30% Systolic blood pressure <100 mmHg Cardiothoracic ratio >55 Creatinine >2·5 mg . dl 1 Ventricular tachycardia ACE-inhibitors Beta-blockers 79·3 28·8 23·9 53·3 53·1 22·7 30·5 2·7 52·2 30·5 27·1 83·6 20·4 mortality and of mortality due to sudden death. A two-tailed P<0·05 was considered statistically significant. Results The study population of 5517 patients had a mean age of 6312 years (range 14–96 years), included 1295 (23·5%) women and 1544 (28·0%) cases of NYHA class III–IV congestive heart failure. The 767 patients with complete 1-year follow-up data who were excluded from the present analysis were of similar age (6512 years; range 17–91 years), with a larger prevalence of women (38·6%, P<0·01) and of NYHA class III–IV congestive heart failure (38·8%, P<0·01). Complete left bundle-branch block and atrial fibrillation: prevalence and associated clinical characteristics Of the 5517 patients included in the present analysis, 3328 (60·3%) had neither left bundle-branch block nor atrial fibrillation (group A), 1206 (21·9%) had an isolated complete left bundle-branch block (group B), 798 (14·5%) had an isolated chronic atrial fibrillation (group C), and 185 (3·3%) had complete left bundle-branch block associated with chronic atrial fibrillation (group D). The demographic and clinical characteristics of the four groups are reported in Table 1. Group D patients were more frequently males and, as a probable result of the presence of chronic atrial fibrillation, group C and D patients were older than those in the other two groups. Patients in group D presented a greater reduction in functional capacity as assessed by NYHA classification, and more significant Eur Heart J, Vol. 23, issue 21, November 2002 69·1 27·7 30·9 33·5 54·8 30·5 49·9 3·3 62·4 49·9 28·2 79·6 13·4 75·2 43·7 36·5 33·3 59·4 20·1 29·6 2·8 67·6 29·6 37·0 87·6 17·2 81·6 44·7 44·9 35·4 67·0 31·9 44·7 7·6 67·6 44·7 30·4 86·5 9·2 0·001 0·001 0·001 0·001 0·001 0·001 0·001 0·001 0·005 0·033 ns 0·001 0·001 clinical impairment as demonstrated by the higher rate of patients with a third heart sound, previous hospitalization for congestive heart failure, hypotension and cardiac enlargement. Groups D and B had more severe left ventricular dysfunction and a higher rate of renal dysfunction. The prevalence of ventricular tachycardia was similar across the four groups. A high proportion of patients presented in each group had been hospitalized for congestive heart failure in the previous year, and this proportion was highest in group D. The prevalence of ischaemic heart disease was significantly higher in group A. ECG abnormalities and prognosis Overall, 659/5517 (11·9%) patients died over the 1-year follow-up, with almost half the deaths (n=306) being classified as sudden. All-cause mortality and mortality due to sudden death was significantly higher among patients with any of the two ECG abnormalities and was highest when these were associated than in the other three groups (Fig. 1). Indeed the contemporary presence of left bundle-branch block and atrial fibrillation was associated with 26·5% 1-year all-cause mortality (unadjusted RR 6·11, 95% CI 3·76–9·90) being 11·2% of all deaths classified as sudden death and 15·3% as non-sudden mortality. Similarly, the prevalence of hospital admissions during follow-up (Fig. 2) was significantly higher in groups B and C than in group A and highest (28·1%) in group D (unadjusted RR 1·83, 95% CI 1·26–2·67). Further analyses were then carried out to predict the adjusted hazard ratio for all-cause death and sudden death at 1 year. In these models, we entered all the variables that in univariate analyses (data not shown) were associated with all-cause mortality (Table 2). Age, Left bundle-branch block associated with atrial fibrillation in CHF patients 1695 effect and, on average, it was estimated to increase the risk of all-cause death at 1 year by 85% (Table 2, Fig. 1). The same variables, with the exclusion of renal failure, were significantly associated with the risk of sudden death at 1 year (Table 3). Also in this multivariate model the contemporary presence of left bundle-branch block and atrial fibrillation was an independent predictor of the risk of sudden death, that was increased by 86% when both ECG abnormalities were present. Discussion Figure 1 One-year total mortality and sudden death in patients without complete left bundle-branch block (LBBB) and chronic atrial fibrillation (AF) (group A), with isolated left bundle-branch block (group B), with isolated chronic atrial fibrillation (group C) and simultaneous presence of complete left bundle-branch block and atrial fibrillation (group D). Relative risk of all-cause P < 0·001 28·1 30 25 % A Unadjusted 1 21·9 21·7 B C D 1·23 1·21 1·83 (1·01– (1·03– (1·26– 1·49) 1·43) 2·67) 20·1 20 18·7 15 10 Other causes of hospitalization Hospitalization for HF 0 AF: LBBB: A – – B – + C + – D + + Total population 5 Figure 2 One-year hospitalization for all-cause and for heart failure (HF) in patients without complete left bundle-branch block (LBBB) and chronic atrial fibrillation (AF) (group A), with isolated left bundle-branch block (group B), with isolated chronic atrial fibrillation (group C) and simultaneous presence of complete left bundlebranch block and atrial fibrillation (group D). heart rate and systolic blood pressure were entered as continuous variables while all the other variables presented in the two tables were entered as dichotomous variables. The risk of all-cause death at 1 year was significantly increased with advancing age and in the presence of ischaemic heart disease, previous hospitalization for congestive heart failure, and several indicators of disease severity or co-morbidity such as NYHA class III–IV, reduced systolic blood pressure, third heart sound, ventricular tachycardia, and renal failure (Table 2). However, even after adjusting for all these covariates, the association of left bundle-branch block with atrial fibrillation still retained its unfavourable prognostic In the last few years, the prognosis of patients with congestive heart failure was largely improved mainly due to the widespread and increasing use of effective therapies such as ACE-inhibitors, beta-blockers and spironolactone[16–20]. However, morbidity and mortality still remain high, suggesting the need to identify subgroups of patients particularly, those at high risk, with the aim of individually tailoring pharmacological therapy or newer nonpharmacological therapeutic strategies, such as multisite cardiac pacing[21]. In keeping with other recent studies, our analysis demonstrated that atrial fibrillation and left bundlebranch block are useful clinical variables with which to identify a population at higher risk of total and sudden death in congestive heart failure[22,23]. In this study we have demonstrated that these two electrical abnormalities have a cumulative, negative effect on the prognosis of patients with congestive heart failure. A further clinically relevant finding of our study was that patients presenting with both left bundle-branch block and atrial fibrillation have an increased risk not only of 1-year total mortality but also of hospitalization, with the consequent increase in the costs to the health care system and the further deterioration of patients’ quality of life. The clinical and demographic profiles of patients with atrial fibrillation and/or left bundle-branch block were different from those of patients without these abnormalities. These patients are older and had several characteristics suggesting a higher degree of clinical and functional impairment. It has been commonly acknowledged that older and sicker patients are often undertreated with evidence-based recommended therapies. For example, advanced age has been shown to be an independent predictor of a reduced prescription rate of ACE-inhibitors or beta-blockers[24–26]. This finding, which may only in part account for the age-associated increase in co-morbidity, can have a dramatic effect on prognosis[24,26]. In the last few years, multisite cardiac and in particular biventricular pacing, was tested and seemed to be effective in treating patients with congestive heart failure associated with a left intraventricular conduction delay. In fact this strategy can improve cardiocirculatory functional reserve and patient’s perceived quality of life[27,28]. Eur Heart J, Vol. 23, issue 21, November 2002 1696 S. Baldasseroni et al. Table 2 Multivariate predictors of 1-year all-cause death in patients with atrial fibrillation or left bundle-branch block and in patients with complete left bundlebranch block associated with atrial fibrillation Variable HR 95% CI P= Age (years)# Ischaemic heart disease (yes vs no) Previous hospitalization for CHF (yes vs no) NYHA (III–IV vs I–II) Systolic blood pressure (mmHg)# Third heart sound (yes vs no) Ventricular tachycardia (yes vs no) Renal failure (yes vs no) LBBB or AF (yes vs no) LBBB and AF (yes vs no) ACE–inhibitors (yes vs no) Beta–blockers (yes vs no) 1·02 1·25 1·75 1·93 0·99 1·42 1·76 1·66 1·32 1·85 0·82 0·75 1·01–1·03 1·05–1·47 1·46–2·09 1·64–2·27 0·98–0·99 1·21–1·68 1·28–2·42 1·06–2·60 1·11–1·56 1·35–2·53 0·68–0·99 0·58–0·96 0·0001 0·0103 0·0001 0·0001 0·0001 0·0001 0·0005 0·0268 0·0013 0·0001 0·0480 0·0248 HR=hazard ratio; #=introduced as continuous variables; AF=atrial fibrillation; LBBB=complete left bundle-branch block. Variables excluded from the model (P>0·10): sex; cardiothoracic ratio; left ventricular ejection fraction. Table 3 Multivariate predictors of 1-year risk of sudden death in patients with atrial fibrillation or left bundle-branch block and in patients with left bundle-branch block associated with atrial fibrillation Variable HR 95% CI P= Age (years)# Ischaemic heart disease (yes vs no) Previous hospitalization for CHF (yes vs no) NYHA (III–IV vs I–II) Systolic blood pressure (mmHg)# Third heart sound (yes vs no) Ventricular tachycardia (yes vs no) LBBB or AF (yes vs no) LBBB and AF (yes vs no) Beta–blockers 1·01 1·32 1·88 1·52 0·99 1·71 1·96 1·35 1·86 1·50 1·00–1·03 1·03–1·69 1·44–2·44 1·19–1·94 0·98–0·99 1·35–2·17 1·25–3·08 1·06–1·73 1·16–2·99 1·03–2·20 0·0100 0·0288 0·0001 0·0007 0·0007 0·0001 0·0034 0·0157 0·0105 0·0351 HR=hazard ratio; #=introduced as continuous variables; AF=atrial fibrillation; LBBB=complete left bundle-branch block. Variables excluded from the model (P>0·10): sex; cardiothoracic ratio; left ventricular ejection fraction; renal failure; ACE-inhibitors. Recently Leclercq et al. have demonstrated that biventricular pacing stimulation was particularly effective in patients with congestive heart failure and wide QRS associated with atrial fibrillation[29]. Other perspectives for patients with left bundlebranch block and atrial fibrillation could derive from a new kind of atrial stimulation. Padeletti et al. have recently demonstrated that inter-atrial septum pacing, after restoration sinus rhythm, reduces the incidence of supraventricular arrhythmic episodes and in particular the relapse of atrial fibrillation[30]. This new technique, in association with biventricular resyncronization, could become, in the near future, another possible method of reducing mortality in patients presenting with both left bundle-branch block and atrial fibrillation. However, the efficacy of this approach in this regard needs to be confirmed by ad-hoc clinical trials of adequate size, because its usefulness is Eur Heart J, Vol. 23, issue 21, November 2002 only supported by preliminary results obtained in small series of patients with ‘soft’ end-points. Our epidemiological data might help identify, in the large heterogeneity of congestive heart failure patients, the small subgroup in which these new pacing techniques might be specifically tested on relevant end-points such as morbidity and mortality. Another relevant finding derived from our study is that we analysed the prognosis of patients who are often excluded from randomized clinical trials in spite of the fact that they represent a consistent part of the congestive heart failure outpatient population with a poor prognosis especially in the elderly. In contrast to a recent study focused in the community setting[31], in our study left bundle-branch block alone or associated with atrial fibrillation is also an independent predictor of a poor prognosis in outpatients. This may have been the result of the strict Left bundle-branch block associated with atrial fibrillation in CHF patients definition of a wide QRS in our study (QRS >120 ms associated with morphological characteristics) in respect of the study by Farwell et al.[31]. Our study also shows that atrial fibrillation alone is likely to be an independent predictor of all-cause deaths in patients affected by congestive heart failure. Some limitations of our study must be acknowledged. Due to the original purpose of the database used for this analysis, examination of ECG measurements of QRS duration was performed locally, albeit by a single, trained cardiologist at each centre with subsequent standardized, blinded methods and quality control techniques in a single core laboratories. Twenty-four hour Holter monitoring to assess the presence of chronic atrial fibrillation was analysed locally by the attending cardiologist. Finally, the multivariate model was adjusted for clinical and demographic variables. With respect to non-cardiac co-morbidities, the model was adjusted only for renal failure, a limitation that becomes particularly important if we consider that older patients present commonly with an increased burden of concomitant non-cardiac diseases that may well affect their overall prognosis. In spite of these limitations, we believe that our analysis provides information useful in identifying a well-defined subgroup of patients at higher risk of death and who deserve specific consideration and even more aggressive treatments to improve their poor prognosis. In this perspective our observations can represent the rationale for future studies aimed at evaluating whether ventricular resynchronization and restoration of sinus rhythm can reduce such an increased risk of mortality. References [1] Kelly DT. Paul Dudley White International Lecture. Our future society. A global challenge. Circulation 1997; 95: 2459–64. [2] Kannel WB, Belanger AJ. Epidemiology of heart failure. Am.Heart J 1991; 121: 951–7. [3] Gillum RF. Epidemiology of heart failure in the United States. Am Heart J 1993; 126: 1042–7. [4] Rich MW. Epidemiology, pathophysiology and etiology of congestive heart failure in older adults. J Am Geriatr Soc 1997; 45: 968–74. [5] Cohn JN, Rector TS. Prognosis of congestive heart failure and predictors of mortality. Am J Cardiol 1988; 62: 25A–25A. [6] Carson P, Johnson G, Fletcher R et al. Mild systolic dysfunction in heart failure (left ventricular ejection fraction >35%): baseline characteristics, prognosis and response to therapy in the Vasodilator in Heart Failure Trials (V-HeFT). J Am Coll Cardiol 1996; 27: 642–9. [7] Opasich C, Pinna GD, Bobbio M, Sisti M et al. Peak exercise oxygen consumption in chronic heart failure: toward efficient use in the individual patient. J Am Coll Cardiol 1998; 15: 776–5. [8] Myers J, Gullestad L, Vagelos R et al. Cardiopulmonary exercise testing and prognosis in severe heart failure: 14 mL/ kg/min revisited. Am Heart J 2000; 139: 78–84. [9] Willenheimer R, Erhardt LR. Value of 6-min-walk test for assessment of severity and prognosis of heart failure. Lancet 2000; 355: 515–16. 1697 [10] Gottipaty V, Krelis S, Lu F et al. The resting electrocardiogram provides a sensitive and inexpensive marker of prognosis in patients with chronic congestive heart failure. J Am Coll Cardiol 1999; 33 (Suppl A): 145A. [11] Scardi S, Mazzone C, Pandullo C et al. Lone atrial fibrillation: prognostic differences between paroxysmal and chronic forms after 10 years of follow-up. Am Heart J 1999; 137: 686–91. [12] Middlekauff HR, Stevenson WG, Stevenson LW. Prognostic significance of atrial fibrillation in advanced heart failure. Circulation 1991; 84: 40–8. [13] Stevenson WG, Stevenson LW, Middlekauff HR et al. Improving survival for patients with atrial fibrillation and advanced heart failure. J Am Coll Cardiol 1996; 28: 1458–63. [14] Opasich C, Tavazzi L, Lucci D et al. Comparison of one-year outcome in women versus men with chronic congestive heart failure. Am J Cardiol 2000; 86: 26–30. [15] The Task Force on Heart Failure of the European Society of Cardiology. Guidelines for the diagnosis of heart failure. Eur Heart J 1995; 16: 741–51. [16] Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitors Trials. JAMA 1995; 273: 1450–6. [17] Packer M, Colucci WS, Sackner-Bernstein JD et al. Doubleblind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. The PRECISE Trial. Prospective Randomized Evaluation of Carvedilol on Symptoms and Exercise. Circulation 1996; 94: 2793. [18] The Cardiac Insufficiency Bisoprolol Study II (CIBIS II). A randomized trial. Lancet 1999; 353 (9146): 9–13. [19] Hjalmarson A, Goldstein S, Fargerberg B et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Interventional Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group. JAMA 2000; 283: 1295–302. [20] Pitt B, Zannadt F, Remme WJ et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999; 341: 709–17. [21] Tavazzi L. Ventricular pacing: a promising new therapeutic strategy in heart failure. For whom? Eur Heart J 2000; 21: 1211–14. [22] Torp-Pedersen C, Moller M, Bloch-Tomsen et al. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group. N Engl J Med 1999; 16: 857–65. [23] Baldasseroni S, Opasich C, Gorini M et al. Complete left bundle-branch block is associated with 1 year mortality in patients with congestive heart failure (CHF): data from INCHF registry. J Am Coll Cardiol 2001; 37: 156A. [24] Havrenek EP, Abrams F, Stevens E et al. Determinants of mortality in the elderly patients with heart failure of angiotensin-converting enzyme inhibitors. Arch Intern Med 1998; 158: 2024–8. [25] Husten L. ATLAS shows global undertreatment of heart failure. Lancet 1998; 351 (9108): 1035. [26] Soumerai SB, McLaughlin TJ, Spiegelman D et al. Adverse outcomes of underuse of betablockers in the elderly survivors of acute myocardial infarction. JAMA 1997; 277: 115–21. [27] Auricchio A, Stellbrink C, Sack S et al. The Pacing Therapies for Congestive Heart Failure (PATH-CHF) study: rationale, design, and endpoints of a prospective randomized multicenter study. Am J Cardiol 1999; 83: 130D–135D. [28] Gras D, Mabo P, Tang T et al. Multisite pacing as a supplemental treatment of congestive heart failure: preliminary results of the Medtronic Inc. InSync Study. Pacing Clin Electrophysiol 1998; 21: 2249–55. [29] Leclercq L, Victor F, Alonso C et al. Comparative effects of permanent biventricular pacing for refractory heart failure in patients with stable sinus rhythm or chronic atrial fibrillation. Am J Cardiol 2000; 85: 1154–6. Eur Heart J, Vol. 23, issue 21, November 2002 1698 S. Baldasseroni et al. [30] Padeletti L, Porciani MC, Michelucci A et al. Interatrial septum pacing: a new approach to prevent recurrent atrial fibrillation. J Interv Card Electrophysiol 1999; 3: 35–43. [31] Farwell D, Patel NR, Hall A et al. How many people with heart failure are appropriate for biventricular resyncronization? Eur Heart J 2000; 21: 1255–9. Appendix Participating Centers and Investigators Piemonte Borgomanero (A. Mezzani, M. Bielli); Cuneo (U. Milanese, G. Ugliengo); Orbassano (R. Pozzi, F. Rabajoli); Veruno (E. Bosimini); Valle d’Aosta Aosta (G. Begliuomini); Lombardia Belgioioso (A. Ferrari, F. Barzizza); Bergamo (M. G. Valsecchi, F. Dadda); Brescia (P. Faggiano); Cassano D’Adda (G. Castiglioni, G. Gibelli); Chiari (A. L. Turelli); Como (R. Belluschi); Cremona (C. Bianchi, C. Emanuelli); Desio (S. Gramenzi, G. Foti); Erba Medicina (D. Agnelli); Esine (G. Mascioli); Garbagnate Milanese (E. Cazzani); Gussago (E. Zanelli, D. Domenighini); Legnano (C. Castelli); Mariano Comense (E. Moroni); Milano Fondazione Don Gnocchi (E. Gara); Milano Osp. Sacco Medicina (S. Guzzetti, S. Muzzupappa, M. Turiel, E. Cappiello, G. Sandrone); Milano Osp. Niguarda II Cardiologia (F. Recalcati); Milano Pio Albergo Trivulzio (D. Valenti); Monza (F. Achilli, A. Vincenzi); Passirana (F. Rusconi, M. Palvarini); Pavia Policlinico San Matteo (S. Ghio, A. Fontana, A. Giusti, L. Scelsi, R. Sebastiani; M. Ceresa); Pavia I.I.A.A.R.R.S. Margherita (A. Ferrari); Saronno (D. Nassiacos, S. Meloni); Seriate (T. Nicoli); Sondalo (P. Bandini); Tradate Fondazione Maugeri (R. Pedretti, M. Paolucci); Tradate Osp. Di Circolo Galmarini (L. Amati, M. Ravetta); Varese Osp. Di Circolo (F. Morandi, S. Provasoli); Varese Osp. Di Circolo Medicina (A. Bertolini, D. Imperiale, W. Agen); Vizzolo Predabissi (E. Planca, P. Quorso); P. A. di Trento Rovereto (A. Ferro); Rovereto Medicina (C. Pedrolli); Veneto Belluno (P. Russo, L. Tarantini); Castelfranco Veneto (G. Candelpergher); Conegliano Veneto (P. P. Cannarozzo); Feltre (F. De Cian, A. Agnoli); Montebelluna (M. G. Stefanini); Padova (L. Cacciavillani, G. M. Boffa); Pieve Di Cadore (L. Mario); Treviso (G. Renosto, P. Stritoni); Vicenza (L. Varotto, M. Penzo); Villafranca (G. Perini); Friuli Venezia Giulia Gorizia (G. Giuliano); Monfalcone (E. Barducci); San Vito al Tagliamento (R. Piazza); Udine Osp. S. M. della Misericordia (M. C. Albanese, C. Fresco); Udine Casa di Cura (F. Picco, P. Venturini); Liguria Arenzano (A. Camerini, R. Griffo); Genova Osp. Galliera (G. Derchi, L. Delfino); Genova-Sestri Ponente (L. Pizzorno); Genova Osp. S. Martino (S. Mazzantini, F. Torre); Rapallo (S. Orlandi); Sarzana (D. Bertoli); Sestri Levante (A. Gentile); Emilia Romagna Bologna Poliambulatorio Tiarini (F. Naccarella, M. Gatti, M. Coluccini); Forlı̀ (G. Morgagni); Modena Osp. Sant’Agostino (G. Alfano); Modena Policlinico (L. Reggianini, S. Sansoni); Parma (W. Serra); Piacenza (F. Passerini); Riccione (P. Del Corso, L. Rusconi); Eur Heart J, Vol. 23, issue 21, November 2002 Rimini (M. Marzaloni, M. Mezzetti), Scandiano (G. P. Gambarati); Toscana Castelnuovo Garfagnana (P. R. Mariani, C. Volterrani); Empoli (F. Venturi); Firenze Osp. S. M. Nuova (G. Zambaldi); Firenze Osp. Nuovo S. Giovanni di Dio (G. Casolo); Firenze Azienda Osp. Careggi (G. Moschi); Fucecchio (A. Geri Brandinelli); Grosseto (G. Miracapillo); Lucca (A. Boni); Pescia (G. Italiani, W. Vergoni); Pisa Osp. Santa Chiara (A. M. Paci); Pontedera (F. Lattanzi, B. Reisenhofer); San Giovanni Valdarno (D. Severini, T. Taddei); Viareggio (A. Dalle Luche, A. Comella); Umbria Foligno (U. Gasperini); Gubbio (M. Cocchieri); Perugia Monteluce (G. Alunni, E. Bosi, R. Panciarola); Spoleto (G. Maragoni, G. Bardelli); Marche Ancona Osp. Sestilli (P. Testarmata); Ancona Osp. Lancisi Centro Medicina Sociale (L. Pasetti, A. Budini); Ancona Osp. Lancisi II Cardiologia (D. Gabrilelli); Camerino (B. Coderoni); Lazio Albano Laziale (P. Midi); Grottaferrata (C. Romaniello); Roma INRCA (D. Del Sindaco, F. Leggio); Roma Osp. Forlanini (A. Terranova); Roma Osp. San Camillo II Cardiologia (G. Pulignano); Roma Osp. San Camillo Servizio (F. Pozzar); Roma Osp S. F. Neri (G. Ansalone, B. Magris, P. Giannantoni); Roma Osp. S. Giovanni (G. Cacciatore, G. Bottero, G. Scaffidi); Roma Osp. Sandro Pertini (C. Valtorta, A. Salustri); Roma Osp. Sant’Eugenio (F. Amaddeo, G. Barbato); Roma Osp. Santo Spirito (N. Aspromonte); Roma Osp. Cristo Re (V. Baldo, E. Baldo); Abruzzo Popoli (C. Frattaroli, A. Mariani); Vasto (G. Di Marco, G. Levantesi); Molise Larino (A. P. Potena), Termoli (N. Colonna, A. Montano); Campania Napoli Osp. Monaldi Medicina (P. Sensale, V. Rullo); Napoli Osp. S. Gennaro (A. Somelli); Nola (F. Napolitano, P. Provvisiero); Oliveto Citra (P. Bottiglieri); Puglia Bari Policlinico (N. Ciriello); Brindisi (E. Angelini, C. Andriulo); Casarano (F. De Santis); Francavilla Fontana (F. Cocco); Galatina Medicina (A. Zecca); Gallipoli (A. Pennetta, F. Mariello); Lecce Osp. Fazzi (F. Magliari, A. De Giorgi, M. Callerame); Mesagne (V. Santoro); San Pietro Vernotico (S. Pede, A. Renna); Scorrano (O. De Donno, E. De Lorenzi); Taranto Osp. SS. Annunziata (G. Polimeni, V. A. Russo); Tricase (R. Mangia); Basilicata Policoro (L. Truncellito); Calabria Belvedere Marittimo (F. P. Cariello); Catanzaro Policlinico Servizio (M. Affinita); Catanzaro Policlinico Divisione (F. Perticone, C. Cloro, D. Borelli); Cetraro (M. Matta, D. Lopresti); Cosenza Osp. Dell’Annunziata (G. Misuraca, R. Caporale); Cosenza Osp. Dell’Annunziata Medicina (P. Chiappetta); Reggio Calabria Osp. Morelli (E. Tripodi, F. Tassone); Rossano (S. Salituri); Siderno (C. Errigo); Trebisacce (G. Meringolo, L. Donnangelo); Sicilia Avola (G. Canonico); Catania Osp. Cannizzaro (R. Coco, M. Franco); Messina Osp. Papardo (A. Coglitore, A. Donato); Messina Osp. Piemonte (G. Di Tano); Messina Policlinico (D. Cento, C. De Gregorio); Palermo Casa Del Sole (M. Mongiovı̀); Palermo Osp. Buccheri La Ferla FBF (A. M. Schillaci); Palermo Osp. Civico (U. Mirto); Palermo Osp. Ingrassia (F. Clemenza); Palermo Villa Sofia (F. Ingrillı̀); Piazza Armerina (A. Cavallaro, B. Aloisi); Trapani (G. Ledda, C. Rizzo); Sardegna Cagliari Brotzu (M. Porcu, S. Salis, L. Pistis); Cagliari Osp. SS. Trinità (G. Pili, S. Piras); Nuoro (I. Maoddi); Sassari (F. Uras).
Scaricare