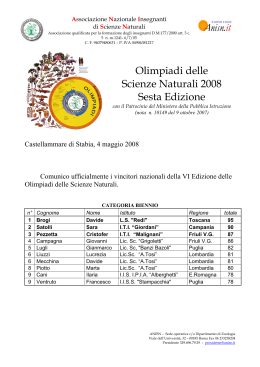
Fourth Mediterranean Congress Innovative Scenario in Internal Medicine Palermo 6-7 june 2014 LA COMPLESSITÀ CLINICA DELL’EMOGLOBINOPATIE NELL’ADULTO M. Domenica Cappellini, M.D. FACP, FRCP Dipartimento di Medicina Interna Fondazione Ca Granda Policlinico IRCCS Universita’ di Milano Disclaimer This presentation reflects only my personal opinion, not that of my employer or faculty, for the purposes of independent scientific discussion and is not intended to promote any product or indication, nor to promote any products of sponsors of this conference. It must not be quoted without my prior written permission. I assert ownership of copyright of this presentation in all countries. The data I present and my views may relate to doses or indications outside of those recommended in medicinal product SmPCs. Please refer to prescribing information and SmPCs in your country of practice for more information 1925: Cooley description 1925: Rietti 1928: Greppi 1880: Cardarelli 1884: Somma 1935: Miceli 1940–1950: Caminopetros, Silvestroni, Bianco Hb abnormalities, hereditary pattern 1960–1970: Weatheral and Clegg Hb chain synthesis 1980–2000: Prenatal diagnosis (Kan) Bone marrow transplantation (Lucarelli) Present: Gene therapy? 1949–1960: Pauling: Hb structure HbS-Mendelian transmission Ceppellini: HbA2 1970–1980: transfusional therapy Iron chelation: deferoxamine 2000… new oral iron chelators ANEMIE CONGENITE:EMOGLOBINOPATIE Varianti Emoglobiniche - > 400 - la maggior prte sono silenti - clinicalmente rilevanti HbS, HbC, HbD - talassemia like: HbE, HbLepore Sindromi Talassemiche - alfa talassemia - beta talassemia TDT and NTDT Miglioramento della sopravvivenza nelle forme di talassemia Trasfusione Dipendenti 1985–1997 1980–1984 1975–1979 1.00 1970–1974 Survival probability 0.75 Birth cohort 0.50 1965–1969 1960–1964 0.25 p < 0.00005 0 0 5 10 15 20 25 30 Age, years DFO, deferoxamine Borgna-Pignatti C, et al. Haematologica. 2004;89:1187-93. MEDIAN PATIENT AGE HAS INCREASED SINCE THE INTRODUCTION OF CHELATION THERAPY Age distribution of β thalassemia patients over several surveys North America Italy/Greece 30 1973 (n=243) Percent of patients 25 1985 (n=303) 20 15 1993 (n=443) 1993 (n=271) 2002 (n=319) 2003 (n=170) 10 5 0 0–5 6–10 11–15 16–20 21–25 26–30 31–35 36–40 41–45 46–50 51–55 Age (years) Vichinsky E P et al. Pediatrics 2005;116:e818-e825. Cross-sectional study; n=781. 6 CLASSIFICAZIONE IN RAPPORTO AL FABBISOGNO TRASFUSIONALE Non-transfusion-dependent thalassaemias (NTDT) β-Thalassaemia intermedia Mild/moderate haemoglobin E/β-thalassaemia α-Thalassaemia intermedia (haemoglobin H disease) TDT Transfusions seldom required Occasional transfusions required (e.g. surgery, pregnancy, infection) Intermittent transfusions required (e.g. poor growth and development, specific morbidities) Regular, lifelong transfusions required for survival α-thalassemia trait β-thalassemia minor β-thalassemia major Severe haemoglobin E/ β-Thalassaemia Α-Thalassaemia major (hemoglobin Bart’s hydrops fetalis) Musallam KM et al. Haematologica 2013;98:833. SOURCE OF COMPLICATIONS Typical disease-related complications • Hepatosplenomegaly • Extramedullary hematopoietic pseudotumours • Bone deformities • Osteoporosis • Gallstones Disease- and iron overload-related complications • Liver complications: • Liver fibrosis • Hepatocellular carcinoma • Pulmonary hypertension • Vascular • Endocrine morbidities • Renal dysfunction • Leg ulcers • Thrombotic events Musallam KM, et al. Haematologica. 2013;98:833-44; Musallam KM, et al. Curr Opin Hematol. 2013;20:187-92. Complicanze cliniche nelle NTDT vs. le TDT β-Thalassaemia major (regularly transfused) NTDT Silent cerebral ischaemia Hypothyroidism Hypoparathyroidism Cardiac siderosis Left-sided heart failure Hepatic failure Viral hepatitis Diabetes mellitus Pulmonary hypertension Right-sided heart failure Extramedullary haemopoietic pseudotumours Hepatic fibrosis, cirrhosis and cancer Gallstones (cholelithiasis) Splenomegaly Hypogonadism Osteoporosis Osteoporosis Venous thrombosis Leg ulcers Musallam KM, et al. Haematologica. In press 2013. FOCUS OF THALASSAEMIA CARE HAS SHIFTED AS TREATMENT IMPROVES 50 anaemia Primary cause of death: Iron overload Others… 45 Number of deathsa 40 35 Unknown 30 Other 25 20 15 10 5 Malignancy Iron overload Infection BMT complication Anaemia 0 The number of deaths in the 2000–2003 interval represents deaths during 4 years; in all the other groups, the number of deaths is over 5 years. a Modell B, et al. J Cardiovasc Magn Reson 2008;10:42. Case-control study; n=1089. Improved survival of -thalassaemia patients in the UK with CMR and modern iron chelation 1970: regular transfusions became the norm 1980: DFO therapy became standard practice 1999 onwards: T2* CMR introduction oral iron chelation 50 45 Unknown Other Malignancy Iron overload Infection BMT complication Anaemia 40 Deaths, n 35 30 25 20 15 10 5 0 1950– 1955– 1960– 1965– 1970– 1975– 1980– 1985– 1990– 1995– 2000– a 1954 1959 1964 1969 1974 1979 1984 1989 1994 1999 2003 a The number of deaths in the 2000–2003 interval represents deaths during 4 years, and in all the other groups the number of deaths is over 5 years. BMT, bone marrow transplantation; CMR, cardiac magnetic resonance; DFO, deferoxamine. Modell B, et al. J Cardiovasc Magn Reson. 2008;10:42. Diversa severità di sovraccarico di ferro cardiaco Carpenter JP, et al. Circulation. 2011;123:1519-28 IRON CHELATORS HAVE BEEN AVAILABLE SINCE THE 1960S 2006 DFX approved by EMEA 1960s DFO came into clinical use 1990s 1960sto 1980s 90 1977 Subcutaneous DFO 92 94 2012 FBS0701 Phase II results 2000s 96 98 00 1999 DFP approved by EMEA DFO, deferoxamine; DFP, deferiprone; DFX, deferasirox; EMEA, European Medicines Agency; FDA, Food and Drug Administration, USA 02 04 2010s 06 2005 DFX approved by FDA 08 10 12 14 2011 DFP approved by FDA OVERVIEW OF IRON CHELATORS: PHARMACOKINETIC PROFILES DFO1 DFP2 DFX3 20–40 mg/kg 75–99 mg/kg 20–40 mg/kg Administration SC (also IV, IM); 8–12 hours, 5–7 days/week Oral; TID Oral; QD Half-life First phase: 1 hour Second phase: 6 hours 2–3 hours 8–16 hours Low Intermediate High Urinary, faecal Urinary Faecal Property Daily dose Lipid solubility4 Excretion Efficiency 10–17% efficient when given at 25–50 mg/kg over 8–10 hours, 5–7 days/week5 4% of administered dose 27% of drug eliminated in eliminated in urine bound to iron iron-bound form when given at at 25 mg/kg/day, TID6 10–30 mg/kg/day, QD5 Please refer to prescribing information in your country of practice. IM, intramuscular; IV, intravenous; QD, once daily; SC, subcutaneous; TID, three times daily • • • • • Desferal (deferoxamine) US Prescribing Information. 2011 FERRIPROX (deferiprone ) US Prescribing Information. 2012 EXJADE (deferasirox) US Prescribing Information. 2013 Porter J et al. Blood 2005;106:abstr 2690 Hoffbrand AV et al. Blood 2003;102:17–24 15 Impact of a decade of cardiac MRI assessment on cardiac T2* Cohort of 132 patients from UCLH/Whittington hospital p < 0.001 Proportion of patients (%) 70 60 60 Baseline Median 9 years follow-up 50 40 30 p < 0.001 23 20 17 10 7 0 T2* ≤ 20 ms T2* < 10 ms Thomas AS, et al. Blood. 2010;116:[abstract 1011]. • Thalassaemia International Federation • www AHA Consensus Statement Cardiovascular Function and Treatment in β-Thalassemia Major:A Consensus Statement From the American Heart Association Dudley J. Pennell, MD, FRCP, FAHA, Co-Chair et al. on behalf of the American Heart Association Committee on Heart Failure and Transplantation of the Council on Clinical Cardiology and Council on Cardiovascular Radiology and Imaging Circulation 2013 Quindi……………….. • I pazienti con TDT saranno sempre più frequentemente ammessi ai DH/reparti di Medicina Interna • Le pluripatologie conseguenza della patologia di base (talassemia) e delle complicanze terapeutiche richiedono la competenza internistica • E’ indispensabile conoscere I meccanismi fisiopatologici del danno d’organo nella talassemia e modulare le terapie di conseguenza • Conoscere I nuovi approcci terapeutici per la ferro chelazione LIVING BETTER: EMERGING IMPORTANCE OF QOL As a result of conventional and novel therapeutic strategies, large majority of TDT patients in the developed world are living better with dramatically improved quality of life1 However, the burden of regular therapy may pose a negative impact on patients’ HR-QoL2 Main impact factors on QoL3,4: Organization of transfusion Start time, availability and compliance with chelation therapy Management of secondary complications Transition from pediatric care to adult services2 Psychological support and communication Cao A. Haematologica. 2004 Oct;89(10):1157-9. Levine L, Levine M. Ann N Y Acad Sci. 2010;1202:244-7. Caocci G, et al. BMC Blood Disorders 2012, 12:6. Telfer P, et al. Ann N Y Acad Sci. 1054: 273–282. HR-QoL, health-related quality of life; TM, thalassemia major. CLASSIFICAZIONE IN RAPPORTO AL FABBISOGNO TRASFUSIONALE Non-transfusion-dependent thalassaemias (NTDT) β-Thalassaemia intermedia Mild/moderate haemoglobin E/β-thalassaemia α-Thalassaemia intermedia (haemoglobin H disease) TDT Transfusions seldom required Occasional transfusions required (e.g. surgery, pregnancy, infection) Intermittent transfusions required (e.g. poor growth and development, specific morbidities) Regular, lifelong transfusions required for survival α-thalassemia trait β-thalassemia minor β-thalassemia major Severe haemoglobin E/ β-Thalassaemia Α-Thalassaemia major (hemoglobin Bart’s hydrops fetalis) Musallam KM et al. Haematologica 2013;98:833. Overview on Practices in Thalassemia Intermedia Management Aiming for Lowering Complication-rates Across a Region of Endemicity: the OPTIMAL CARE study Parameter Age (years) < 18 18–35 > 35 Male:female Splenectomized Serum ferritin (µg/L) < 1,000 1,000–2,500 > 2,500 Frequency n (%) 172 (29.5 ) 288 (49.3) N = 127 124 (21.2) KM Musallam 291 (49.8) : 293 (50.2) AT Taher 325 (55.7) 376 (64.4) 179 (30.6) 29 (5) Complications Osteoporosis EMH Hypogonadism Cholelithiasis Thrombosis PHT Abnormal liver function Leg ulcers Hypothyroidism Heart failure Diabetes mellitus EMH, extramedullary haemopoiesis. Cross-sectional study of 584 β-TI patients from 6 comprehensive care centres in the Middle East and Italy 134 (22.9) 124 (21.2) 101 (17.3) 100 (17.1) 82 (14) 64 (11) 57 (9.8) 46 (7.9) 33 (5.7) 25 (4.3) 10 (1.7) N = 200 M Karimi N = 12 S Daar N = 153 MD Cappellini N = 51 A El-Beshlawy N = 41 K Belhou Taher AT, et al. Blood. 2010;115:1886-92. Complicanze cliniche nelle NTDT vs. le TDT β-Thalassaemia major (regularly transfused) NTDT Silent cerebral ischaemia Hypothyroidism Hypoparathyroidism Cardiac siderosis Left-sided heart failure Hepatic failure Viral hepatitis Diabetes mellitus Pulmonary hypertension Right-sided heart failure Extramedullary haemopoietic pseudotumours Hepatic fibrosis, cirrhosis and cancer Gallstones (cholelithiasis) Splenomegaly Hypogonadism Osteoporosis Osteoporosis Venous thrombosis Leg ulcers Musallam KM, et al. Haematologica. In press 2013. Le complicanze nelle NTDT aumentano con l’età ≤ 10 years 45 * 21–32 years 35 Frequenza (%) > 32 years 120 pazienti naïve ad ogni terapia 40.0 40 11–20 years 33.3 * 30.0 30 * * 26.7 26.7 25 * 20.0 20.0 20 16.7 15 23.3 23.3 * 16.7 16.7 13.3 13.3 13.3 10.0 10 6.7 5 0 20.0 20.0 6.7 3.3 10.0 6.7 3.3 3.3 6.7 3.3 0 13.3 10.0 16.7 13.3 10.0 10.0 6.7 3.3 16.7 6.7 3.3 0 0 3.3 0 0 *Statistically significant trend. ALF, abnormal liver function; DM, diabetes mellitus; HF, heart failure. Taher A, et al. Br J Haematol. 2010;150:480-97. Le complicanze nelle NTDT aumentano con l’età ≤ 10 years 45 * 21–32 years 35 Frequenza (%) > 32 years 120 pazienti naïve ad ogni terapia 40.0 40 11–20 years 33.3 * 30.0 30 * * 26.7 26.7 25 Le Complicanze nelle NTDT aumentano con l’età * 20 * e compaiono generalmente dopo la prima decade 15 di vita 10 23.3 23.3 20.0 20.0 16.7 16.7 16.7 13.3 13.3 13.3 10.0 6.7 5 0 20.0 20.0 6.7 3.3 10.0 6.7 3.3 3.3 6.7 3.3 0 13.3 10.0 16.7 13.3 10.0 10.0 6.7 3.3 16.7 6.7 3.3 0 0 3.3 0 0 *Statistically significant trend. ALF, abnormal liver function; DM, diabetes mellitus; HF, heart failure. Taher A, et al. Br J Haematol. 2010;150:480-97. La ferritina sottostima il sovraccarico di ferro nelle NTDT β-TI Linear (β-TI) Serum ferritin level (μg/L) 10,000 β-TM Linear (β-TM) 8,000 6,000 4,000 LIC values in β-TI were similar to those in β-TM, but serum ferritin levels were significantly lower 2,000 0 0 5 10 15 20 25 30 35 40 45 50 LIC (mg Fe/g dry wt) LIC, liver iron concentration. Musallam KM, Taher AT. N Engl J Med. 2011;364:1476. Taher A, et al. Haematologica. 2008;93:1584-6. ANALISI ROC: FERRITINA PUO’ ESSERA UTILIZZATA PER STIMARE APPROSSIMATIVAMENTE LA CONCENTRAZIONE EPATICA DI FERRO (LIC) ROC curve for using serum ferritin to predict LIC ≥ 5 mg Fe/g dw based on patients screened for entry to THALASSA Patients with SF >800 ng/mL had a high probability of LIC ≥5 mg Fe/g dw SF >2,000 ng/mL was highly predictive of LIC ≥7 mg Fe/g dw SF ≤300 ng/mL appears adequate and safe to interrupt deferasirox therapy ROC, receiver operating characteristic Taher AT et al. Haematologica IRON OVERLOAD AND MORBIDITIES LIC (mg Fe/g dry wt) 21 p = 0.490 p = 0.027 p = 0.002 p < 0.001 p = 0.245 p < 0.001 p = 0.682 p = 0.040 p < 0.001 p < 0.001 168 non-chelated β-TI 18 Morbidity absent 15 Morbidity present 12 9 6 3 0 Musallam KM et al. Haematologica 2011;96:1605 IRON OVERLOAD AND MORBIDITIES LIC (mg Fe/g dry wt) 21 p = 0.490 p = 0.027 p = 0.002 p < 0.001 p = 0.245 p < 0.001 p = 0.682 p = 0.040 p < 0.001 p < 0.001 168 non-chelated β-TI 18 Morbidity absent 15 Morbidity present On multivariate analysis, a 1 mg Fe/g dry wt increase in LIC was significantly associated with higher odds of thrombosis, PHT, hypothyroidism, osteoporosis, and hypogonadism 9 12 6 3 Adjusted for age, gender, splenectomy status, transfusion history, total haemoglobin level, foetal haemoglobin level, platelet count, nucleated RBC count, and serum ferritin level 0 Musallam KM et al. Haematologica 2011;96:1605 LIVER COMPLICATIONS IRON OVERLOAD AND THE LIVER Several case reports and case series suggest an association between iron overload and hepatocellular carcinoma in hepatitis C negative patients with NTDT HCV Plus iron 1.Maakaron JE, et al. Ann Hepatol. 2013;12:142-6. 2.Maakaron JE, et al. Br J Haematol. 2013;161:1.. 3.Restivo Pantalone G, et al. Br J Haematol. 2010;150:245-7. 4.Borgna-Pignatti C, et al. Br J Haematol. 2004;124:114-7. 5.Mancuso A. World J Hepatol. 2010;2:171-4. HEPATOCELLULAR CARCINOMA OCCURRING ON NON-VIRAL, NON-CIRRHOTIC LIVERS Sex Age* Survival HCV Ab HCV RNA HBV Ab HBs Ag AFP (kU/L) Serum ferritin (μg/L) Ferritin peak (μg/L) LIC M 48 Alive at 26 m - - - - 2851 1,520 5,250 NA F 61 5m - - - 132 369 6,000 NA F 59 25 m + - NA NA NA 990 NA NA M 73 7m - - NA NA NA 574 NA NA M 54 1m - - - - 17.8 1,291 2,490 12.3 M 51 4y - - Vaccinated - 3.8 5,602 7,138 23.9 + *At diagnosis In 6 β-TI patients with HCC who were HCV- and HBV-negative, no parameter was consistently elevated or depressed Suggested screening algorithm for HCC in β-TI – measure LIC using non-invasive R2* MRI yearly – if LIC ≥ 5 mg Fe/g dry wt, screen for HCC using abdominal ultrasound every 6 months Ab = antibody; AFP = alpha-fetoprotein; HBV = hepatitis B virus; LIC = liver iron concentration; MRI = magnetic resonance imaging; NA = not available. Maakaron JE, et al. Ann Hepatol. 2013;12:142-6. RENAL DISFUNCTIONS 48% had evidence of glomerular hyperfiltration 14% patients had proteinuria* patients had elevated LIC > 7 mg Fe/g dry wt, NTBI, and nucleated RBC counts UPr/UCr ratio (mg/g) RENAL DYSFUNCTION IN Β-TI IS ASSOCIATED WITH IRON OVERLOAD 1,800 1,600 1,400 1,200 1,000 800 600 400 200 0 rs = 0.357 p = 0.011 A considerable proportion of patients showed evidence of abnormally elevated eGFR, with a declining trend towards advancing age Occurrence of proteinuria associated with anaemia, haemolysis and iron toxicity • *UPr/UCr ratio > 500 mg/g UPr/UCr ratio (mg/g) 0 5 10 15 20 25 30 LIC (mg Fe/g dry wt) 1,800 1,600 1,400 1,200 1,000 800 600 400 200 0 35 rs = 0.444 p = 0.001 -4 -2 0 2 4 BTBI (µmol/L) • 6 8 10 N = 50 Ziyadeh FN et al. Nephron Clin Prac 2012;121:c136 MECHANISMS OF RENAL DISEASE IN -TI Glomerular filtration rate (GFR) Chronic anaemia / hypoxia Iron overload Iron chelation ? Renal plasma flow Vascular resistance GFR Endothelial and epithelial damage Transudation of macromolecules Mesangial dysfunction GFR Chronic anaemia/hypoxia Relative iron depletion Abnormal mitochondrial function and arachidonic acid cascade Tubuloglomerular feedback and haemodynamic change Tubular cell damage Epithelial-mesenchymal transdifferentiation Tubulointerstitial injury Glomerular sclerosis GFR GFR Tubular cells Iron overload Oxidative stress Lipid peroxidation Cellular damage Iron chelation Nephrotoxicity Musallam KM et al. J Am Soc Nephrol 2012;23:1299 EXTRAMEDULLARY HAEMATOPOIETIC PSEUDOTUMOURS EXTRAMEDULLARY HAEMOPOIETIC PSEUDOTUMOURS IN β-TI Chronic anaemia and hypoxia Increased bone marrow haemopoietic activity and expansion + Formation of erythropoietic tissue masses around the body Symptoms develop due to pressure on surrounding structures Spinal cord compression and possible irreversible neurological damage most serious Haidar R et al. Eur Spine J 2010;19:871 PULMONARY & CARDIAC HYPERTENSION (PHT & CHT) Prevalence and Risk Factors for Pulmonary Arterial Hypertension in a Large Group of b-Thalassemia Patients Using Right Heart Catheterization: a Webthal Study Giorgio Derchi, Renzo Galanello, Patrizio Bina, Maria Domenica Cappellini, Antonio Piga, Maria-Eliana Lai, Antonella Quarta, Gavino Casu, Silverio Perrotta, Valeria Pinto, Khaled M.Musallam and Gian Luca Forni Circulation. published online September 30, 2013; PULMONARY HYPERTENSION IN β-TI Not correlated with age or Hb level, in contrast to previously reported data Not correlated with ferritin level – implies that ferritin testing is useless in predicting PHT LIC (mg Fe/g dw) Significantly correlated with LIC 5000 40 30 r=0.514 P=0.01 4000 3000 20 2000 r=0.097 P=0.513 10 1000 Serum ferritin (ng/mL) PHT (defined as PASP ≥30 mm Hg) present in 38.5% 0 0 60 20 40 80 Tricuspid gradient (mm Hg) Serum ferritin LIC TCG and SF TCG and LIC LIC, liver iron concentration; PASP, pulmonary artery systolic pressure Isma’eel H et al. Am J Cardiol 2008;102:363 VASCULA COMPLICATIONS FACTORS CONTRIBUTING TO HYPERCOAGULABLE STATE IN β-TI Transfusion ↑ Splenectomy Iron overload ↑ ↑ ↑ ↑ Red blood cells Endothelial injury Platelets ↑ Thrombin generation (phosphatidyl serine exposure) ↑ Rigidity, deformability, and aggregation Expression of adhesion molecules and tissue factor Thrombocytosis Chronic activation ↑ Adhesion and aggregation ↑ Circulating microparticles ↓ Antithrombin III ↓ Protein C ↓ Protein S Endocrine & hepatic dysfunction ?↑ Atherosclerosis THROMBOSIS Taher AT et al. TIF Guidelines 2013; Musallam KM et al. Haematologica 2013 Jun;98(6):833-44. VASCULAR COMPLICATIONS IN NTDT Incidence data are limited: Venous -thal major1 -TI1 Splenectomized -TI2 Number of patients Incidence 683 52 83 4% 9.6% 29% 4.4 more frequent than in -thal major 14% -TI3 8,860 -TI4 584 Cerebrovascular -TI5 -TI6 Splenectomized -TI7 HbE / -thalassaemia8 16 30 30 37.5% 60% 26.7% 24% Taher AT et al. TIF Guidelines 2013; 1Borgna Pignatti C et al. Acta Haematol 1998;99:76-79; 2Cappellini MD et al. Br J Haematol 2000;111:467-473; 3Taher AT et al. Thromb Haemost 2006;96:488-491; 4Taher AT et al. Blood 2010;115:1886-1892; 5Manfre L et al. AJR Am J Roentgenol 1999;173:1477-1480; 6Taher AT et al. J Thromb Haemost 2010;8:54-59; 7Karimi M et al. Thromb Haemost 2010;103:989-993; 8Metarugcheep P et al. J Med Assoc Thai 2008;91:889-894. THROMBOEMBOLIC EVENTS IN A LARGE COHORT OF β-TI PATIENTS 146 (1.65%) thrombotic events β-TM: 61/6,670 (0.9%) β-TI: 85/2,190 (3.9%) Age (> 20 years) Previous thromboembolic event Family history Splenectomy 66 Stroke Type of event 48 Venous Risk factors for developing thrombosis in β-TI 28 9 Iron chelation Hydroxyurea 23 DVT 39 8 PE Transfusion 12 11 PVT 0 8 Others 12 0 0.56 0.28 6.59 Splenectomy 19 STP 0.97 20 30 40 TM (n = 61) TI (n = 85) SF ≥ 1,000 μg/L Hb ≥ 9 g/dL Female Age > 35 years 60 Thromboembolic events (%) DVT, deep vein thrombosis; PE, pulmonary embolism; PVT, portal vein thrombosis; SF, serum ferritin; STP, superficial thrombophlebitis. 80 1.86 0.41 1.27 2.59 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Adjustedodds odds ratio thrombosis Adjusted ratioforfor thrombosis Musallam K et al. Hemoglobin 2011;35:503 Taher A et al. Thromb Haemost 2006;96:488 Ferro chelazione nelle NTDT • La ferro-chelazione ha un effetto protettivo verso Ipertensione polmonare, colelitiasi e osteoporosi The OPTIMAL CARE study* Complication RR 95% CI PHT Cholelithiasis Hypogonadism Osteoporosis 0.53 0.30 2.51 0.40 0.29–0.95 0.18–0.51 1.48–4.26 0.24–0.68 p value 0.032 < 0.001 0.001 0.001 Taher AT, et al. Blood. 2010;115:1886-92. Altre opzioni terapeutiche per complicanze specifiche Complicazione Opzioni Terapeutiche PHT – Sildenafil citrato, bosentan ( Masse di eritropoiesi extramidollare – – – Radiazioni chirurgia Idrossiurea Osteopenia/osteoporosi – – – Ca++, Vit D, altre misure di prevenzione ?Bisfosfonati Trattare le endocrinopatie Endocrinopatie – Terapie sostitutive Trombosi e vasculopatia cerebrale – – Antiaggreganti, anticoagulanti(no clinical trials) Risk-assessment models Ulcere arti inferiori – – Ipertrasfusione Fattori di crescita locali Musallam KM, et al. Cold Spring Harb Perspect Med. 2012;2:a013482. Taher AT, et al. Br J Haematol. 2011;152:512-23. The compilation of the results has just been published Per concludere…………. La sopravvivenza dei pazienti affetti da sindromi talassemiche (TDT e NTDT) è significativamente aumentata La morbidità aumenta significativamente con l’età L’interessamento multiorgano e la pluriterapia richiede competenze internistiche Le competenze internistiche devono essere integrate alla conoscenza delle basi fisiopatologiche delle sindromi talassemiche L’interazione medico/paziente/ infermiere è essenziale per un outcome clinico positivo
Scaricare