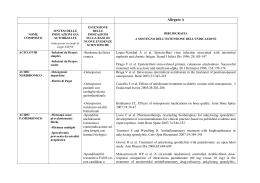
La Terapia nelle Spondiloartriti Carlo Salvarani, Unità Operativa di Reumatologia, Ospedale di Reggio Emilia Terapia nelle SpA SPONDILITE ANCHILOSANTE ARTROPATIA PSORIASICA Spondilite Anchilosante La storia naturale della spondilite anchilosante: uno studio prospettico Studio prospettico di 150 veterani americani con SA iniziato nel 1947 81 erano ancora vivi nel 1980 ed erano stati rivisti periodicamente 51 /81 erano rivalutati (durata media SA: 38 anni) 21 (41%) progressione a severa limitazione della mobilità della colonna 81% di questi 21 pts presentavano una severa limitazione già nei primi 10 anni di malattia Carrette et al, Arthr Rheum, 1983 The Natural Course of Radiographic Progression in AS – Evidence for Major Individual Variations in a Large Proportion of Patients Baraliakos et al, J Rheumatol 2009 March 30 (Epub ahead of print) Objective: to describe the natural course of radiographic progression Methods: 146 patients with AS who had never received TNF-blockers and had complete sets of cervical and lumbar radiographs from at least 2 timepoints within 6 years The Natural Course of Radiographic Progression in AS – Evidence for Major Individual Variations in a Large Proportion of Patients Baraliakos et al, J Rheumatol 2009 March 30 (Epub ahead of print) Results: - 43% of patients showed a 4-fold greater rate of progression than the mean - 23% had no progression - the number of syndesmophytes at baseline predicted the radiographic progression Spine x-rays syndesmophytes ASAS/EULAR Recommendations for the Management of AS Zochling et al, Ann Rheum Dis 2006 there is no evidence for the efficacy of disease modifying antireumatic drugs (DMARDs), including sulfasalazine and methotrexate, for the treatment of axial disease. Sulfasalazine may be considered in patients with peripheral arthritis NELLA SPONDILITE ANCHILOSANTE VI E’ LA NECESSITA’ DI TRATTAMENTI: - efficaci sulle manifestazioni assiali (e anche su quelle periferiche e extra-articolari) - in grado nel lungo termine di funzionare come agenti modificanti la malattia Malattia di Chron associata con SA Efficacia della terapia anti-TNF con infliximab in pazienti con malattia di Crohn e sintomi articolari (n = 4) Van den Bosch et al, Lancet 2000 Pathology – TNF and AS Increased TNF serum levels in AS patients Gratacos J, et al. Br J Rheumatol 1994; 33:927-931 Increased TNF mRNA and protein in biopsy specimens from inflamed SI joints of patients with AS Braun J et al, Arthritis Rheum 1995; 38(4):499-505 Adalimumab, etanercept and infliximab for the treatment of AS: a systematic review and economic evaluation McLeod C, et al. Health Technol Assess 2007; Review The review of clinical data related to the 3 drugs compared with conventional treatment plus placebo indicates that in the short term (12-24 weeks), the 3 treatments are clinically effective in relation to assessment of ASAS, BASDAI and BASFI Indirect comparisons of treatments did not show a significant difference in effectiveness between the 3 agents Argomenti Mantenimento dell’efficacia e sicurezza nel trattamento prolungato anti-TNF Cosa succede alla sospensione dell’agente anti-TNF? Sicurezza e efficacia della ripresa della terapia anti-TNF E’ la terapia anti-TNF in grado di inibire il danno strutturale? Mantenimento dell’efficacia nel trattamento prolungato Braun J et al. Persistent clinical efficacy and safety of anti-TNFα therapy with infliximab in patients with AS over 5 years – evidence for different types of response. Ann Rheum Dis 2008 Davis Jr JC, et al. Efficacy and safety of up to 192 weeks of etanercept therapy in patients with AS. Ann Rheum Dis 2008 van der Heijde D, et al. Adalimumab treatment maintains efficacy and safety in patients with AS – 2 year results from ATLAS. Ann Rheum Dis 2008 Sicurezza nel lungo termine Only 2 patients (4.6%) in infliximab therapy discontinued the study for possibly drug-related events (recurrent vaginal and upper respiratory tract infections) Only 4 patients (1.6%) during long-term etanercept therapy had infections leading to study withdrawal Only 6 patients (1.9%) during long-term adalimumab therapy had serious infections leading to study withdrawal Real life experience confirms sustained response to long-term biologics and switching in AS Coates et al, Rheumatology 2008 Treatment of active AS with TNF blockers according to the BSR guidelines leads to a sustained response for over 2 yrs with most patients tolerating the drugs well The rate of non-response is significantly lower than that seen in RA and nearly all of these patients respond well to a second-line agent Cosa succede alla sospensione della terapia anti-TNF? Brandt J, et al. Six-month results of a doubleblind, placebo-controlled trial of etanercept treatment in patients with active AS. Arthritis Rheum 2003 Baraliakos X, et al. Clinical response to discontinuation of anti-TNF therapy in patients with AS after 3 years of continuous treatment with infliximab. Arthritis Res Ther 2005 Cosa succede alla sospensione della terapia anti-TNF? comparsa di recidiva (incremento di almeno 2 nel BASDAI) nel 75% dei pazienti entro 3 mesi dalla sospensione di etanercept (media 6 settimane) recidiva di malattia più tardiva nel restante 25% dei pazienti Brandt J et al, Arthritis Rheum 2003 Cosa succede alla sospensione della terapia anti-TNF? Il 98% dei pazienti con SA che sospendevano infliximab dopo 3 anni di terapia continuativa avevano un recidiva (BASDAI > 4) entro 52 settimane dalla sospensione e dovevano essere ritrattati Il tempo medio di recidiva dalla sospensione della terapia era 17,5 settimane Baraliakos X et al, Arthritis Res Ther 2005 Sicurezza e efficacia della ripresa della terapia anti-TNF Dopo 24 e 48 settimane di risomministrazione di infliximab i valori di BASDAI erano simili ai quelli di prima della sospensione La incidenza globale di effetti collaterali era simile a quella dei primi 3 anni di terapia negli stessi pazienti Baraliakos X et al, J Rheumatol 2007 TNF-blockers and MRI in AS Adalimumab, etanercept and infliximab significantly reduce both spinal and SI joint inflammation in patients with active AS, and these improvements are maintained during the treatment Lambert, et al. Arthritis Rheum 2007 Marzo-Ortega H, et al. Arthritis Rheum 2001 Braun J, et al. Arthritis Rheum 2003 E’ in grado il trattamento continuativo di ridurre o bloccare il danno strutturale (evoluzione radiologica) Baraliakos X, et al. Outcome of patients with active AS after 2 years of therapy with etanercept: clinical and MRI data. Arthritis Rheum 2005 Van der Heijde D, et al. Two-year etanercept therapy does not inhibit radiographic progression in patients with AS. Ann Rheum Dis 2006 Baraliakos X, et al. Radiographic progression in patients with AS after 4 yrs of treatment with anti-TNF-α antibody infliximab. Rheumatology 2007 Van der Heijde D, et al. Radiographic findings following two years of infliximab therapy in patients with AS. Arthritis Rheum 2008 E’ in grado il trattamento continuativo di ridurre o bloccare il danno strutturale (evoluzione radiologica) MRI evaluation showed a 75% improvement of active spinal lesions, but minor spinal inflammation was still present in 64% of patients after 2 years of therapy with etanercept Whereas clinical findings demonstrate sustained, durable benefits with long-term (2 years) etanercept therapy, x ray evaluations (cervical and lumbar spine scored with mSASSS) suggest that progression of structural damage continued Baraliakos X, et al. Arthritis Rheum 2005 Van der Heijde D, et al. Ann Rheum Dis 2006 E’ in grado il trattamento continuativo di ridurre o bloccare il danno strutturale (evoluzione radiologica) There is some radiographic progression after 2 and 4 years of infliximab therapy in AS patients (cervical and lumbar spine scored with mSASSS) AS patients who received infliximab from baseline through week 96 did not show a statistically significant difference in inhibition of structural damage progression at year 2, as assessed using the mSASSS scoring system, when compared with radiographic data from the historical control OASIS cohort Baraliakos X, et al. Rheumatology 2007 Van der Heijde D, et al. Arthritis Rheum 2008 AS and RA: TNF-blocker therapy and radiographic progression In RA the proinflammatory effects of TNF coincide with osteoclast activation and subsequent bone erosion In RA there is a clear longitudinal relationship between clinical disease activity and subsequent radiographic damage The hallmark of AS is bone formation rather than bone resorption Schett G et al. Ann Rheum Dis 2007; Welsin PM et al. Arthritis Rheum 2004; Van der Heijde D et al, Arthritis Rheum 2008 AS and RA: TNF-blocker therapy and radiographic progression Structural progression in AS seems to be independent of TNF, despite the fact TNF is responsible for inflammatory signs/symptoms In AS there is no relationship between radiographic progression and clinical disease activity Schett G et al. Ann Rheum Dis 2007; Welsin PM et al. Arthritis Rheum 2004; Van der Heijde D et al, Arthritis Rheum 2008 Possible Explanations for the Lack of TNF-blockers Efficacy on Radiographic Progression in AS The average disease duration of TNF-blockers treated AS patients in the studies was ~ 10 years Earlier intervention in the disease process, before the reparative processes have started, could prevent further bone formation Inflammation would have to be suppressed for a longer period of time before the inhibitory effects can be seen on radiographs Van der Heijde et al, Arthritis Rheum 2008 Artrite Psoriasica TERAPIA DELL ’ARTROPATIA PSORIASICA DELL’ARTROPATIA l’AP non è una malattia più lieve della AR: 40% dei pts ha una malattia erosiva e deformante in uno studio della durata di 5 anni la frequenza dei pts con danno radiologico in 5 o più articolazioni passava dal 19% al 41%, nonostante la riduzione della VES e del numero delle articolazioni dolenti/tumefatte Gladman et al, Q J Med 1987 and J Rheumatol 1990 TERAPIA DELL ’ARTROPATIA PSORIASICA DELL’ARTROPATIA l’AP non è una malattia più lieve della AR: Utilizzando il metodo di Steinbroker modificato la severità radiologica dei pazienti con AR era simile a quella dei pazienti con AP quando venivano comparati pazienti di età, sesso e durata di malattia uguale Rahman et al, J Rheumatol 2001 A prospective, clinical and radiological study of early PsA: an early synovitis clinic experience Kane et al, Rheumatology 2003 Objective: to determine the clinical presentation and clinical and radiological outcome of early PsA (disease duration < 2 years) at 1 and 2 years Despite clinical improvement with current DMARDs, PsA resulted in radiological damage in up to 47% of patients at a median interval of 2 years PsA is a chronic, progressive disease in the majority of patients Terapia dell’artropatia psoriasica i DMARDs tradizionali controllano i sintomi, ma non vi sono dimostrazioni che siano in grado di inibire il danno articolare strutturale Gli agenti anti-TNFα riducono i segni/sintomi, migliorano lo stato funzionale e la qualità della vita e inibiscono la progressione del danno strutturale nell’artrite periferica Risks and benefits of TNF-α inhibitors in the management of PsA: systematic review and metaanalysis of RCTs Saad AA, et al. J Rheumatol 2008 6 RCT (982 patients) of adalimumab, etanercept, and infliximab used in PsA patients were identified All 3 drugs were significantly more effective than placebo on the basis of PsARC, ACR20, ACR50, and ACR70 All 3 drugs blocked radiographic progression All 3 drugs were shown to be equally effective in the treatment of PsA There was no differences between these 3 drugs and placebo in the proportions of patients experiencing withdrawal for any reason or due to adeverse events, and serious adverse events Mease PJ et al. ADEPT 1699 # A25 S. Diego ACR 2005 Mean Change in mTSS Mean change in mTSS through Week 48 1,5 Placebo eow Adalimumab 40 mg eow 1 0,5 * 0 -0,5 0 Placebo Adalimumab 24 N Baseline Week 24 mean change 141 133 22.1 23.4 0.9 –0.1 *p<0.001, adalimumab (Week 48) vs placebo (Week 24) 48 Week 48 mean change 1.0 0.1 Cost-effectiveness of etanercept and adalimumab in psoriatic arthritis: the Italian studies adalimumab appears to be cost effective for the treatment of PsA Eandi and Salvarani, Farmeconomia e percorsi terapeutici 2006 TNF antagonists (mainly etanercept) provide “value” and “value for money” in the treatment of PsA in clinical practice Olivieri et al, Rheumatology 2008 Frequency and duration of clinical remission in patients with peripheral psoriatic arthritis requiring second-line drugs Cantini F et al, Rheumatology 2008 Remission is possible in up to 24% of patients with peripheral PsA It is significantly more frequent, but not longer, in patients receiving anti-TNF drugs compared with those treated with traditional DMARDs Patients remain in remission for a long period after therapy interruption, thus suggesting an intermittent therapeutic strategy Systematic review of treatments for psoriatic arthritis: an evidence based approach and basis for treatment guidelines Kavanaugh AF, Ritchlin CT, and the GRAPPA Treatment Guideline Committee J Rheumatol 2006; 33:1417-21 PsA: management Diagnosis Monoarthritis Tenosyinovitis Local therapy NSAIDs Low-dose CS Asymmetric Oligoarthritis Local therapy NSAIDs Low-dose CS ≥5 joints >ESR PsA spondylitis DMARDs ASAS guidelines Nonresponders PsA: traditional DMARDs therapy DMARD PARENTERAL GOLD RETINOIDS ANTIMALARIAL AGENTS SULFASALAZINE METHOTREXATE CYCLOSPORIN A LEFLUNOMIDE Meta -analisi dei trials controllati e randomizzati per Meta-analisi valutare ll’efficacia ’efficacia e la tossicit à delle terapie della AP tossicità le due sole terapia di dimostrata efficacia erano la sulfasalazina e le alte dosi di metotressato le basse dosi di metotressato e l’etretinato potrebbero essere efficaci, però i dati disponibili sono insufficienti miglioramento anche del gruppo trattato con placebo Jones et al, Br J Rheumatol 1997 Parenteral gold, Retinoids, Antimalarials 9Parenteral Gold: no evidence of efficacy on arthritis, psoriasis worsening Gladman DD, Semin Arthritis Rheum 2003 9Chloroquine, Hydroxychloroquine: no efficacy Gladman DD, et al. J Rheumatol 1992 9Retinoids: efficacy on psoriasis, slight efficacy on arthritis, frequent AEs Klinkhoff AV, et al. J Rheumatol 1989 TERAPIA CON SSZ NELLA AP in 6 studi randomizzati, doppio cieco, placebocontrollati la sulfasalazina era superiore al placebo nella terapia della AP in uno studio su 221 pts con AP la risposta al trattamento era del 57,8% nel gruppo trattato con SSZ e del 44,6% nel gruppo placebo (p = 0,05) Clegg et al, Arthritis Rheum 1996 TERAPIA CON SSZ NELLA AP mentre la SSZ è efficace nell’artrite periferica, non lo è sulle manifestazioni assiali Dougados et al, Arthritis Rheum 1995 Clegg et al, Arthritis Rheum 1999 non è in grado di rallentare/bloccare la progressione radiologica Rahman et al, J Rheumatol 1998 TERAPIA CON CsA NELLA AP nel 1980 sono comparse descrizioni di casi di psoriasi trattati con CsA in cui vi era miglioramento della artrite associata successivamente sono comparsi numerosi studi aperti che hanno evidenziato l’efficacia della CsA nella AP in uno studio controllato su 35 pts con AP la CsA e il MTX era ugualmente efficaci Spadaro et al, Clin Exp Rheumatol 1995 Salvarani et al, Clin Exp Rheumatol 2002 TERAPIA CON CsA NELLA AP su 170 pts trattati con CsA in 16 studi solo il 6% sospendeva il farmaco per nefrotossicità Olivieri et al, Semin Arthritis Rheum 1997 TERAPIA CON CsA NELLA AP è efficace nella artrite periferica è più efficace della SSZ non vi sono dati sulla sua efficacia nella malattia assiale non vi sono dati sulla sua efficacia sulla progressione del danno radiologico è un terapia sicura Salvarani et al, Clin Exp Rheumatol 2002 Salvarani et al, J Rheumatol 2001 Artrite psoriasica: terapia con MTX 1. 2. 3. Black RL, et al. Methotrexate therapy in psoriatic arthritis. Doubleblind study on 21 patients. JAMA 1964. 21 p., MTX 1-3 mg/Kg ogni 10 gg. (3 iniezioni): riduzione significativa del n° di art. dolenti e tumefatte, miglioramento range art. movimento e riduzione della VES. Pancitopenia 7 p Willkens RF, et al. Randomized, double-blind, placebo controlled trial of low-dose pulse methotrexate in psoriatic arthritis. Arthritis Rheum 1984. 37 p.; studio prospettico di 12 settimane; MTX 7,5-15 mg/sett.. Nessuna differenza significativa per: n° di art. dolenti e tumefatte, rigidità mattutina, psoriasi. VMAM (medico): miglioramento significativo (p=0,001). Nessun evento avverso severo Abu-Shakra M, et al. Longterm methotrexate therapy in psoriatic arthritis: clinical and radiological outcome. J Rheumatol 1995. studio retrospettivo, caso-controllo, durata 24 mesi: 23/38 p.; simile efficacia su risposta clinica e danno radiologico TERAPIA CON MTX NELLA AP è efficace nella artrite periferica non è più efficace delle altre terapie di fondo (?) non vi sono dati sulla sua efficacia nella malattia assiale Salvarani et al, Clin Exp Rheumatol 2002 TERAPIA CON MTX NELLA AP non è probabilmente efficace sulla progressione del danno radiologico (?) è un terapia sicura non vi sono dati sufficienti per valutarne l’efficacia è in corso uno studio controllato, multicentrico inglese Salvarani et al, Clin Exp Rheumatol 2002 Leflunomide nell’Artrite nell’Artrite Psoriasica I risultati di un RCT evidenziano che leflunomide: è efficace sull’artrite periferica, e sulle lesioni cutanee è ben tollerata migliora la qualità della vita non vi sono dati sulla sua efficacia nella malattia assiale e sulla progressione del danno radiologico Kaltwasser J. P. et al. Arthritis & Rheumatism 2004. Recommendations of the Italian Society of Rheumatology for the use of biologic (TNF-α blocking) agents in the treatment of psoriatic arthritis C Salvarani, I Olivieri, N Pipitone, F Cantini, A Marchesoni, L Punzi, R Scarpa, M Matucci-Cerinic Clin Exp Rheumatol 2006 PsA with peripheral arthritis Anti-TNF-α therapy should be considered if: They have not responded to full therapeutic or tolerated doses (unless contraindicated) of at least 2 NSAIDs over 3 months, to at least two steroid injections (in cases of monoor oligoarthritis) as well as to at least two of the DMARDs most commonly used in PsA (methotrexate, ciclosporin, sulfasalazine, leflunomide), administered alone or in combination for at least three months (we consider “full therapeutic doses” 2-3 grams per day for sulfasalazine, 20 mg per week for methotrexate, 3-5 mg per kg/body weight per day for ciclosporin, and 20 mg per day for leflunomide) The Challenge of Early Diagnosis of PsA As in RA, the use of anti-TNFα agents only after failure of traditional DMARDs in PsA will probably change in the near future, since early intervention should be the most effective clinical strategy in PsA Olivieri I et al, J Rheumatol 2008 Effects of TNF-α blockade on metabolic syndrome components in PsO and PsA and additional lessons learned from RA Channual et al, Dermatologic Therapy 2009 MetS is a cluster of several interrelated cardiometabolic risk factors: central obesity, atherogenic dyslipidemia, hypertension, and impaired glucose tolerance PsO and PsA patients are highly predisposed to MetS, diabetes and cardiovascular disease TNF-blockers improve insuline resistance and sensitivity in PsO and PsA The effects of TNF-blockers on blood lipids in PsO and PsA patients are presently unclear Effects of TNF-α blockade on metabolic syndrome components in PsO and PsA and additional lessons learned from RA Channual et al, Dermatologic Therapy 2009 Long term study show statistically significant weight gain and an increase in BMI after TNFblockade in PsO and PsA patients TNF-blockers may improve cardiometabolic risk in PsO and PsA patients reducing systemic inflammation (reduction in IL-6, TNF-α and CRP) and improving endothelial function Effects of etanercept in patients with the metabolic syndrome Bernestein et al, Arch Intern Med 2006 Study: RCTs on patients with MetS alone treated with etanercept for 4 weeks Results: Significant decrease in IL-6, >2 mg/L reduction in CRP, increase in adinopectin (an insulin sensitizer)
Scaricare