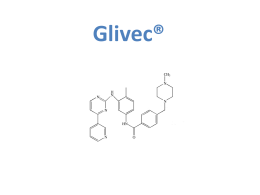
LMC Ph+: introduzione alla patologia, diagnosi, sintesi delle linee guida, stato dell’arte e network internazionali Mario Tiribelli Clinica Ematologica di Udine LMC in fase cronica: presentazione clinica Asintomatica nel 50% dei casi Sintomatologia clinica Astenia Febbricola Perdita di peso/anoressia Senso di distensione addominale Laboratorio Leucocitosi Piastrinosi Faderl S et al, Ann Intern Med 1999; 131:207-219 Goldman JM, Curr Opin Hematol 1997; 4:277-285 Obiettività clinica Splenomegalia LMC: le 3 fasi del decorso clinico Fase cronica Durata media 4-6 anni Fase avanzata Accelerata Fase blastica Durata media sino a 1 anno Sopravvivenza media 3-6 mesi Leucemia mieloide cronica – Sospetto diagnostico leucocitosi con neutrofilia (soprattutto se GB > 20.000 /cc) presenza di cellule immature circolanti (mieloblasti, metamielociti) aumento di basofili e talora eosinofili piastrinosi (30%) splenomegalia Il Cromosoma Philadelphia: la causa della malattia Traslocazione reciproca t(9;22)(q34;q11) t = translocation q = long arm of chromosom Proteina di fusione BCR/ABL con attività tirosin-chinasica che rappresenta la causa della LMC Tutto parte da qui.. E arriva qui.. BCR- ABL PATHWAYS ACTIVATED BY BCR-ABL EXPRESSION RAS BCR/ABL Increased mitogenic signal NUCLEUS F-actin Paxillin ABL Cell Cycle Changes in adhesion to stromal layer Inhibition of apoptosis Decreased normal ABL function at nuclear level: genomic instability Leucemia mieloide cronica… l’inevitabile destino senza terapia.. Fase cronica Fase accelerata Crisi blastica leucemia mieloide cronica terapia Fase cronica Fase accelerata Crisi blastica „il nulla“ LEUCEMIA : tappe della evoluzione della terapia leucemia (1850) tempo chemioterapia (1950) Ph1 (1960) tanto… Trapianto IFN BCR/ABL PCR Imatinib (studio IRIS) Nuovi inibitori TK 11 ALLOGENEIC TRANSPLANT IN CML (THE SEATTLE EXPERIENCE) Doney K et al.: Treatment of chronic granulocytic leukemia by chemotherapy, total body irradiation and allogeneic bone marrow transplantation. Exp Hematol 6, 1978, 738-747. Clift and Storb, BMT 1996 SOPRAVVIVENZA IFN vs CHT STI 571 - Imatinib (Glivec) Classe: 2-fenilaminopirimidin-derivato Peso Molecolare: 590 Da Imatinib: la prima terapia mirata Druker et al. N Engl J Med (2006) 355: 2408-17 ICSG. N Engl J Med (1994) 330: 820-25 Incidence of CCyR, MMR and CMR (undetectable bcr-abl at 4.5 log) with Imatinib – the MDACC experience Kantarjian et al. Cancer 2008 . 12-Month Landmark Analysis - Hammersmith 96% 74% n = 121 n = 72 de Lavallade H et al. JCO 2008;26:3358-3363 Routine Methods for Monitoring CML Disease Burden There are 3 routine methods for measuring CML disease burden: Hematologic response (HR) 1) Measure of blood counts and differentials 1 2 Cytogenetic Response (CyR) 2) Chromosome-banding analysis of marrow cell metaphases Molecular response (MR) 3) Measurement of BCR-ABL transcript levels relative to a control gene 3 Correlation Between Response and Disease Burden Among Detection Methods Number of Leukemic Cells 1012 1010 109 108 107 106 Cytogenetic BCR-ABL Transcripts (log10) 1011 Hematologic Dx CHR (< 1-log) CCyR (2-log) RQ-PCR MMR (3-log) ≈ 5-log reduction Time BCR-ABL levels measured via RQ-PCR correlate with standard HR and CyR criteria1-3 RQ-PCR provides ≥ 3-log greater assay sensitivity than cytogenetics1 CHR, complete HR; Dx, diagnosis; MMR, major MR; RQ-PCR, real-time quantitative polymerase chain reaction. 1. Radich JP. Blood. 2009;114:3376-3381; 2. Baccarani M, et al. Blood. 2006;108:1809-1820; 3. Cross NC, et al. Blood. 1993;82:1929-1936 Glivec… va bene per tutti? 60% Obiettivo raggiunto 40% Risultato non soddisfacente 8% Intolleranza 17% Resistenza 15% Perdita risposta Resistance to treatment Primary resistance – patient fails to achieve a desired response to initial treatment Secondary resistance – patient with an initial response to a TKI ultimately relapses Optimal Response & Time Limit to Achieve it Hematological 1 month CHR Cytogenetic 3 - 6 months CCyR Molecular 12 (??) months MMR Time from start of therapy European LeukemiaNet 2013 recommendations OPTIMAL Baseline NA WARNING - High risk (Sokal, Euro, Eutos) - CCA/Ph+ (major route) FAILURE NA 3 months - BCR-ABL ≤ 10% and/or - Ph+ ≤ 35% - BCR-ABL > 10% and/or - Ph+ 36-95% - No CHR and/or - Ph+ > 95% 6 months - BCR-ABL < 1% and/or - Ph+ 0% - BCR-ABL 1-10% and/or - Ph+ 1-35% - BCR-ABL > 10% and/or - Ph+ > 35% - BCR-ABL >0.1-1% - BCR-ABL > 1% and/or - Ph+ > 0% 12 months - BCR-ABL ≤ 0.1% CCA, clonal cytogenetic abnormalities; CHR, complete hematologic response. Baccarani et al. Blood 2013;122:885-892. BCR-ABLIS<9.8% in 211/279 pts (76%) BCR-ABLIS<10% in 501/692 pts (72%) I farmaci di nuova generazione per la LMC Inibitori tirosin chinasi di seconda generazione Piu potenti di imatinib Efficaci nelle mutazioni resistenti a imatinib Profili di tossicità differenti da imatinib Diagnosi Resistenza o intolleranza o Gli inibitori di seconda generazione sono in grado di produrre una risposta efficace in circa il 50% dei pazienti resistenti o intolleranti a imatinib diagnosi Resistenza o intolleranza o BELA Study Design Phase 3 open-label trial in newly diagnosed CP CML N = 502 139 sites 31 countries Randomization is stratified based on Sokal risk score and geographical regions. R A N D O M I Z E Bosutinib 500 mg/day n = 250 8-year follow-up Imatinib 400 mg/day n = 252 8-year follow-up 1-year analysis • Key eligibility criteria: cytogenetic diagnosis of Philadelphia chromosome–positive (Ph+) CP CML £6 mo prior, no prior therapy other than hydroxyurea or anagrelide • Primary endpoint: complete cytogenetic response (CCyR) at 12 months Cortes J, ASH 2011 BELA – CCyR Rates at Specified Times on Therapy: ITT Population Responders (%) 100 Bosutinib 79% 80% Imatinib 80 * 60 * 50% 70% 68% 63% 59% 62% 67% 55% 65% 58% 49% 40 25% 20 0 3 months 6 months 9 months 12 months 18 months 24 months *Indicates a P value <0.05, which was considered statistically significant. P values at all time points with the exception of at Month 12 were considered exploratory. Cumulative by 24 months BELA – Rates of Treatment Failure: ITT Population Patients (%) 15 Bosutinib 13% Imatinib 10 5 5% 5% 4% 3% 2% 0 a Treatment failure Transformation to AP/BP Overall deaths AP, accelerated phase; BP blast phase. aTreatment failure/disease progression includes both on-treatment transformation to AP/BP and lack of efficacy. BELA – Treatment-emergent Adverse Events Reported for ³ 10% of Patients: Safety Population Bosutinib (n = 248) Adverse event, n (%) Diarrhea Vomiting Nausea Rash Pyrexia Upper abdominal pain Abdominal pain Headache Fatigue Upper respiratory tract infection Cough Arthralgia Myalgia Muscle cramps Bone pain Peripheral edema Periorbital edema All grades 173 (70) 80 (32) 80 (32) 59 (24) 45 (18) 35 (14) 33 (13) 32 (13) 32 (13) 29 (12) 23 (9) 18 (7) 14 (6) 11 (4) 10 (4) 9 (4) 3 (1) Selected adverse events seen more frequently with bosutinib. Selected adverse events seen more frequently with imatinib. Grade 3/4 29 (12) 8 (3) 2 (1) 4 (2) 3 (1) 0 3 (1) 2 (1) 3 (1) 0 0 0 0 0 0 0 0 Imatinib (n = 251) All grades 62 (25) 39 (16) 91 (36) 47 (19) 31 (12) 18 (7) 17 (7) 28 (11) 34 (14) 20 (8) 27 (11) 31 (12) 30 (12) 56 (22) 26 (10) 28 (11) 37 (15) Grade 3/4 2 (1) 0 1 (<1) 2 (1) 3 (1) 0 1 (<1) 0 2 (1) 0 0 1 (<1) 2 (1) 0 2 (1) 0 0 Dasatinib and Nilotinib in de-novo CML DASISION 1,2 ENESTnd 3,4 Dasatinib 100 mg QD Imatinib 400 mg QD Nilotinib 300 mg BID Imatinib 400 mg QD BCR-ABL ≤ 10%IS at 3 mo. 84% 63% 90.7% 66.7% CCyR by 1 year 83% 72% 80% 65% MMR by 2 years 64% 46% 71% 44% MR4.5 by 4 years 40% 23% 34% 21% 4-yrs rate of progression to accelerated / blastic phase 3.1% 5.4% 0.7% 4.2% 92.9% 92.1% 93.6% 91.6% 4-yrs survival Data from different studies. No direct comparison between dasatinib or nilotinib is possible or suggested. 1 Kantarjian et al. N Engl J Med 2010;362:2260-2270. 2 Cortes et al. ASH 2013 3 Saglio et al. N Engl J Med 2010;362:2251-2259. 4 Saglio et al. ASH 2013. Cumulative incidence of MMR and MR4.5 with frontline Nilotinib and Dasatinib Giles F et al., EJCI 2012 MR4.5 può essere un preditore di sopravvivenza La MR4.5 a 4 anni è stata associata ad una significativamente maggiore probabilità di OS rispetto alla CCR (8 anni OS, 92% contro 83%). Hehlman et al, JCO 2013 The evolution of treatment goals in CML The evolution of treatment in CML 1960 1970 Best expected response 1980 1990 2000 2010 Hydroxyurea IFN Imatinib Nilotinib Nilotinib Dasatinib Complete hematologic response (CHR) Complete cytogenetic response (CCyR) Major molecular response (MMR) Earlier and Deeper Deeper molecular molecular responses responses Tumor Reductiona ! 10% " 1-log ! 1% " 2-log ! 0.1%IS " 3-log Tumor Burden a Compared with baseline levels. ! 0.01%IS " 4-log ! 0.0032%IS " 4.5-log ! 0.0001%IS " 5-log CMR4 and beyond Come valutare il paziente alla diagnosi? Su quali elementi basare la scelta della terapia di prima linea? The evolution of treatment goals in CML The evolution of treatment in CML 1960 1970 Best expected response 1980 1990 2000 2010 Hydroxyurea IFN Imatinib Nilotinib Nilotinib Dasatinib Complete hematologic response (CHR) Complete cytogenetic response (CCyR) Major molecular response (MMR) Earlier and Deeper Deeper molecular molecular responses responses Tumor Reductiona ! 10% " 1-log ! 1% " 2-log ! 0.1%IS " 3-log ! 0.01%IS " 4-log ! 0.0032%IS " 4.5-log ! 0.0001%IS " 5-log Tumor Burden CMR4 and beyond SURVIVAL a Compared with baseline levels. CURE? Achieving Deeper Molecular Responses May Be the First Step to Treatment-Free Remission Response at Time of TKI Discontinuation Patients With Molecular and/or Cytogenetic Relapse, % CCyR2 100% MMR5 100% MMR, CCyR, MCyR6 100% DMR for ≥ 2 years on imatinib1,3,7,8 1. Mahon FX, et al. Lancet Oncol. 2010;11:1029-1035. 2. Goh H-G, et al. Leuk Lymphoma. 2009;50:944-951. 3. Goh H-G, et al. Blood. 2011;118:1189 [abstract 2763]. 4. Rea D, et al. Blood. 2011;118:277 [abstract 604]. ~30%-65% 5. Koskenvesa P, et al. Blood. 2008;112:738 [abstract 2121]. 6. Kuwabara A, et al. Blood. 2010;116:1014-1016. 7. Rousselot P, et al. Blood. 2011;118:1615 [abstract 3781]. 8. Matsuki E, et al. Blood. 2011;118:1607-1608 [abstract 3765]. STIM1: Patients With Sustained CMR on Imatinib Can Maintain TFR Results for principal objective: Estimated rate of TFR at 6 months was 45% (95% CI, 34-55)1 After a median follow-up of 55 mo, molecular relapse had occurred in 61 patients2 • 58 relapses occurred during the first 7 mo • 3 late relapses occurred at mo 19, 20 and 22 Survival Without CML Treatment 100 Estimated TFR at 60 months: 90 80 40% (95% CI, 30%-49%) 70 60 50 40 30 20 10 0 0 6 12 18 24 30 36 42 48 54 60 66 72 78 Months Since Discontinuation of Imatinib STIM1 provided the first demonstration of the feasibility of TFR following TKI therapy in a large cohort of patients with sustained deep molecular response 1. Mahon FX, et al. Lancet Oncol. 2010;11:1029-1035. 2. Mahon FX, et al. Blood. 2013;122(21):[abstract 255]. È possibile aumentare i pazienti eleggibili per il TFR? 100 Nilotinib 300 mg BID (n = 282) Nilotinib 400 mg BID (n = 281) Imatinib 400 mg QD (n = 283) 90 Patients With MR4.5, % 80 70 By 5 Yearsa By 4 Yearsa 60 54%, P < .0001 By 1 50 Yeara 40 30 11%, P < .0001 40%, P < .0001 52%, P < .0001 37%, P = .0002 Δ 21% to 23% 20 Δ 6% to 10% 10 31% Δ 14% to 17% 23% 7%, P < .0001 1% 0 0 1 2 3 4 5 6 Time Since Randomization, Calendar Years No patient who achieved MR4.5 on any arm progressed to AP/BC MR4.5, molecular response ≥ 4.5-logs (BCR-ABLIS ≤ 0.0032%). a Cumulative response rates reported consider each year to consist of twelve 28-day cycles. Saglio G, et al. Blood. 2013:[abstract 92]. CML and the PATH TO CURE Coming back to the new ELN recommendations… OPTIMAL WARNING FAILURE 3 months - BCR-ABL ≤ 10% and/or - Ph+ ≤ 35% - BCR-ABL > 10% and/or - Ph+ 36-95% - No CHR and/or - Ph+ > 95% 6 months - BCR-ABL < 1% and/or - Ph+ 0% - BCR-ABL 1-10% and/or - Ph+ 1-35% - BCR-ABL > 10% and/or - Ph+ > 35% IF several studies have reported that a BCR-ABL >10% at 3 months is associated with an inferior survival, WHY was that BCR-ABL level not taken as an indication of failure mandating a change of therapy? Not only the level but also the dynamics! BCR-ABL %IS CCyR MMR Baseline 3° month 6° month 9° month 12° month Overall survival according to the RELATIVE* BCR-ABL reduction within 3 months *These results are expressed as BCR-ABL/GUS ratio Hanfstein et al. EHA 2013
Scaricare