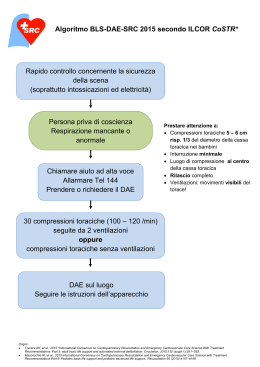
Workshop: Pediatric Advanced Life Support American Heart Association Hotel delle Terme Napoli 22 settembre 2012 RAZIONALE: L’assistenza al bambino critico richiede una precoce decisione delle priorità di intervento che comprendono la classificazione della gravità e la stabilizzazione delle condizioni cliniche del bambino, perché in età pediatrica l’evoluzione clinica delle patologie acute è solitamente più rapida rispetto all’adulto sia in senso migliorativo a fronte di adeguati ed efficaci manovre o procedure sia in senso peggiorativo qualora gli interventi non siano appropriati e precoci. Il Pediatric Life Support base ed avanzato (PALS) riguarda il primo approccio diagnostico-terapeutico fino alla stabilizzazione o alle fasi del trasporto per un bambino critico equivalente ad un’emergenza pediatrica intra o extra ospedaliera. Il corso infatti aumenta le competenze del sanitario nella valutazione e gestione di un lattante o di un bambino con compromissione respiratoria, compromissione circolatoria o arresto cardiaco ) in accordo con le linee guida internazionali e nazionali (ILCOR 2010, AHA e SIMEUP). Il corso si propone di fornire ai partecipanti le conoscenze teoriche, le abilità pratiche e le competenze relazionali e comunicative per il lavoro in team riguardo la gestione delle emergenza pediatriche più frequenti PROGRAMMA 8.30 – 8.45 8.45 – 9.00 Registrazione Partecipanti. Saluti e inizio lavori I SESIONE: LA SIMEUP E LE NUOVE LINEE GUIDA Presidente: F. Esposito Moderatori: D. Perri – V. Tipo – G. Vetrano 09.00 – 09.20 Piano Formativo SIMEUP - Dott. G. Messi 09.20 – 09.40 La manovra per la vita: le iniziative nazionali SIMEUP – Dott. A. Urbino 09.40 – 10.00 dall’ABC al CAB – Dott. R. Lubrano 10.00 – 10.20 NIV in acuto in pazienti neurologici: pro e contro - Dott. R. Falsaperla 10.20 – 11.00 Discussione 11.00 – 11.30 Coffee break II SESIONE: STRUTTURAZIONE DEL PIANO FORMATIVO AHA Presidente: A. Correra Moderatori: R. Cinelli – E. Pianese – R. Vitiello 11.30 – 11.50 BLS per i pediatri – Dott. M. Berg 11.50 – 12.20 ALS per i pediatri – Dott. A. De Caen 12.20 – 12.40 Discussione 12.40 – 14.00 Lunch III SESIONE: LA STABILIZZAZIONE POST ARRESTO DEL BAMBINO CRITICO Presidente: F. Saitta Moderatori: F. Nunziata – M. Ummarino – P. Vairo 14.00 – 14.30 Stabilizzazione post arresto – Dott. C. Cecchetti 14.30 – 15.00 L’ipotermia – Dott. M. Berg 15.00 – 16.00 Teamwork - Dott. A. De Caen 16.00 – 16.30 Discussione 16.30 - 17.00 Chiusura dei lavori e compilazione questionario ECM CURRICULA Antonio Francesco Urbino DATI ANAGRAFICI Cognome URBINO Nome Codice Fiscale RBNNNF56R04E716K AREE DI INTERESSE PREVALENTE ANTONIO FRANCESCO Anno di nascita 1956 (massimo 3 Es.: allergologia, neonatologia, emergenze, qualità, ecc.) PEDIATRIA EMERGENZA RIANIMAZIONE QUALIFICA PROFESSIONALE universitario altro ospedaliero SI pediatra di famiglia medicina dei servizi (specificare) APPARTENENZA A SOCIETA’ SCIENTIFICHE 1) SIP 3) IRC 2) SIMEUP TITOLI DI STUDIO Laurea MEDICINA E CHIRURGIA Conseguita in data 4-11-1981 Specializzazioni PEDIATRIA Conseguita in data 16-7-1986 ESPERIENZE FORMATIVE NAZIONALI ED INTERNAZIONALI ha svolto in qualità di “direttore di corso” circa 300 corsi di BLD esecutori, BLS istruttori, BLSD esecutori, PBLS esecutori, PBLS istruttori, PALS, PALS ISTRUTTORI nell’ambito dell’attivita’ formativa organizzata dalle societa’ scientifiche IRC e SIMEUP ATTIVITA’ SCIENTIFICA Articoli su riviste nazionali (numero) Contributi a libri (numero) Contributi a siti web (numero) 35 Articoli su riviste internazionali 11 Contributi a riviste (numero) 10 Contributi a supporti multimediali 1 (numero) (numero) 10 8 ATTIVITA’ DIDATTICA Insegnamenti universitari : PEDIATRIA D’URGENZA presso Università degli Studi di Torino: Corso di Laurea Infermieristica Pediatrica, Scuola di specializzazione in Pediatria, Scuola di specializzazione in Medicina d’Urgenza ordinario associato ricercatore professore a contratto si Altri insegnamenti ISTRUTTORE SIMEUP DI PBLS, FORMATORE DI FORMATORI DI BASE, ISTRUTTORE SIMEUP DI PALS, FORMATORE DI FORMATORI AVANZATI ISTRUTTORE PALS American Heart Association Tutor di rete SI Animatore di formazione SI ATTIVITA’ LAVORATIVE Attuali Dal 10-12-2007 Direttore della Struttura Complessa di Pediatria d’Urgenza presso l’Ospedale Infantile Regina Margherita (OIRM) di Torino Responsabile del centro di Riferimento Nazionale PBLS ed emergenze pediatriche dell’OIRM di Torino Vicepresidente del Consiglio Direttivo Nazionale della SIMEUP con l’incarico di Responsabile delle Sezioni Regionali Membro del Comitato Tecnico Scientifico corso di formazione specifica in medicina generale della regione Piemonte Pregresse Tirocinio Pratico Ospedaliero nella disciplina di Pediatria dall’1 marzo 1982 al 31 agosto 1982 con giudizio finale di " ottimo". Servizio militare, di Ufficiale medico, presso l'Ospedale Militare di Torino. E' stato inoltre richiamato, in qualità di Ufficiale medico, dal 15 al 31 maggio 1988. Servizio di Guardia Medica, per un numero complessivo di 3456 ore Attività di Pediatra come sostituto di pediatri di libera scelta dall’1982 al 1987 Servizio di Guardia pediatrica notturna e festiva presso la Croce Verde di Torino dal 1982 al 1987 Pediatra di libera scelta a Settimo Torinese dal 1987 al 1991 Da marzo 1980 a giugno 1988 ha frequentato l'Istituto di Clinica Pediatrica dell'Università di Torino In particolare ha svolto attività clinica e di ricerca sul diabete mellito insulinodipendente nel bambino, interessandosi della prevenzione delle complicanze precoci e tardive di tale patologia. Ha inoltre svolto studi sulla diagnosi precoce e sulla terapia delle principali malattie del metabolismo glicolipo-proteico. Durante tale periodo si è altresì interessato allo studio dell'obesità infantile e, in collaborazione con il gruppo di ricerca del dr. Garay dell'ospedale Necker di Parigi, ha svolto, presso il laboratorio dell’ospedale S.Giovanni Bosco di Torino, attività di ricerca inerente i meccanismi di trasporto ionico negli eritrociti dei bambini obesi Titolare, per due anni, di una borsa di studio della Regione Piemonte per lo studio dell’ipertensione in età pediatrica. Coordinatore Nazionale della Commissione PBLS della Medicina d'Urgenza Pediatrica (SIMEUP) e dell’Italian Resuscitation Counceling (IRC) dal settembre 1999 a dicembre 2004 Membro della Commissione Nazionale PALS della SIMEUP dal 1999 al 2004 Consigliere della sezione regionale (Piemonte e Valle d’Aosta) della SIMEUP dal 2000 al 2003 Coordinatore Nazionale della Commissione Formazione della SIMEUP da gennaio 2005 a ottobre 2006 Consigliere del Consiglio Direttivo Regionale (Piemonte e Valle d’Aosta) della SIP dal 2008 al 2011 Coordinatore del Comitato Scientifico del 6° Convegno Nazionale SIMEUP Coordinatore del Comitato Scientifico del 8° Convegno Nazionale SIMEUP Assistente Medico di Pediatria ad Orbassano dal 24-9-87 all’11-1-88 Dirigente medico di I livello presso la Divisione di Pediatria e Neonatologia dell'Ospedale Martini di Torino dal luglio 1988 a dicembre 2007. Negli ultimi anni si è occupato dei problemi dell'emergenza pediatrica e in particolare, dopo essere diventato istruttore di BLS (Basic Life Support) per adulti e istruttore di BLS Pediatrico (PBLS), ha creato, nell'ambito dell'ASL 2, uno dei quattro Centri Pilota Italiani di BLS pediatrico (PBLS). Nell'ambito di tale attività ha eseguito numerosi Corsi di PBLS come istruttore e molteplici " supervisioni" permettendo la nascita di Centri di formazione nazionali PBLS in Sardegna, Campania, Basilicata e Piemonte. Invitato, in qualità di relatore, a molti Congressi sull'urgenza in Pediatria, Da 1-2-2001 è stato nominato coordinatore della SPES (Scuola Permanente Emergenza Sanitaria), istituita dall’ASL 2 per svolgere corsi aziendali a personale interno ed esterno sull’emergenza sia degli adulti che dei bambini. I corsi tenuti dalla SPES sono di BLS esecutore laici e sanitari, BLSD esecutore per sanitari, BLS e BLSD istruttore, DP esecutore, DP istruttore, ACLS esecutore, PBLS esecutore per laici e sanitari, PBLS istruttore, PALS esecutore. Dal 1 giugno 02 a novembre 2004 Direttore della Struttura Semplice di Assistenza neonatale. Nel novembre 2004 a dicembre 2007 Direttore della Struttura Semplice Dipartimentale di “Pediatria di Comunità”. ALTRE NOTIZIE Dal 2002 “Tutor” nel Corso di formazione in Medicina Generale della Regione Piemonte (DM 23-12-97); tale ruolo lo ha impegnato nel seguire la formazione dei giovani medici con quotidiana attività d’insegnamento e d’affiancamento. Da aprile 2009 membro della Commissione “Formazione specifica in medicina generale: programmazione e contenuti formativi” dell’Ordine dei medici di Torino. Autorizzo il trattamento dei miei dati personali ai sensi del Decreto Legislativo 30 giugno 2003, n. 196 "Codice in materia di protezione dei dati personali". Riccardo Lubrano Il Dott. Riccardo Lubrano é nato a Roma il 9.4.1957. Laureato in Medicina e Chirurgia, il 28.07.1981 con votazione di 110/110 e lode . Specializzato in Pediatria, il 09.07.1985 con votazione di 70/70 e lode . Perfezionato in Neonatologia, nell'anno accademico 1985/1986. Specializzato in Nefrologia, il 31.10.1991 con votazione di 70/70 e lode. Specializzato in Anestesia e Rianimazione il 11.10.2005 con votazione di 70/70 e lode Ha conseguito il 26 /10/ 1995, il titolo di Dottore di Ricerca in Scienze Pediatriche Dal 02.11.1995 il dott. Lubrano é in servizio presso il Dipartimento di Pediatria dell'Università degli Studi di Roma "La Sapienza " con la qualifica di Ricercatore ove è responsabile del servizio di Nefrologia Dialisi e Trapianto Pediatrico. Dal 2006 è professore aggregato di pediatria. E’ istruttore PBLSD SIMEUP e Formatore per Formatori E’ istruttore PALS AHA E’ il Responsabile del centro di Formazione SIMEUP presso la propria Università Fa parte inoltre del Centro per la Valutazione e la Promozione della Qualità in Medicina dell’Università degli Studi di Roma “la Sapienza” di cui è stato nell’anno accademico 2008/2009 uno dei professori fondatori, in tale ambito è il responsabile della Simulazione. Il dott. Lubrano e' stato invitato in qualità di relatore a 120 tra congressi e corsi di aggiornamento ove ha trattato prevalentemente di argomenti di nefrologia pediatrica e neonatale e di emergenze pediatriche Ha partecipato alla stesura di 6 testi di pediatria occupandosi di volta in volta della stesura dei capitoli di nefrologia pediatrica e neonatale e di emergenza pediatrica. Attualmente riveste i seguenti incarichi di insegnamento: - Insegnamento di Pediatria del corso di laurea in Medicina e Chirurgia CCLM C - Insegnamento di Pediatria nell’ambito del corso di Medicina d’Urgenza del corso di laurea in Medicina e Chirurgia CCLMC - Insegnamento di Pediatria nell’ambito del corso di laurea per fisioterapisti - Insegnamento di Nefrologia Pediatrica nell’ambito della II scuola di specializzazione in pediatria - Insegnamento di Nefrologia Clinica in Età Pediatrica nell’ambito della I scuola di specializzazione in Nefrologia - Insegnamento di Pediatria d’urgenza nell’ambito del Master in area critica per Infermieri professionali - Insegnamento di Pediatria nell’ambito del master di Medicina d’Urgenza Nell’anno accademico 2009/2010 e 2010/2011 nell’ambito dell’attività scientifica svolta nel Centro per la Valutazione e la Promozione della qualità in medicina ha realizzato un DVD e un libretto esplicativo sulle manovre di base di rianimazione del lattante, del bambino e dell’adulto che sarà distribuito con un corso teorico pratico a tutti gli studenti del I anno della nostra facoltà di Medicina e Chirurgia. Attività nelle società scientifiche - Socio della Società Italiana di Pediatria - Socio della Società Italiana di Emergenza ed Urgenza pediatrica - Socio della Società Italiana di Nefrologia Pediatrica - Socio dell International Society of Pediatric Nephrology Inoltre all’interno delle società scientifiche pediatriche svolge i seguenti incarichi: - Nell’ambito della SIP cura l’aggiornamento scientifico degli iscritti attraverso la realizzazione mensili di Podcast visibili e scaricabili dal sito web della società. - Dal novembre 2009 è tra i direttori responsabili del sito web della Società Italiana di Pediatria - È il segretario della commissione del gruppo di lavoro per le cure semiintensive in pediatria della SIP e ha realizzato la consensus conference sull’argomento che si è tenuta al congresso nazionale di Genova 2008. - Il dott Lubrano è per il triennio 2008 – 2010 è il presidente della SIMEUP Lazio ( società italiana di medicina di emergenza ed urgenza pediatrica ) - Nella stessa società è stato il responsabile dell’attività scientifica dal 2001 al 2007. - Dal 2009 è il responsabile nazionale della formazione della società di Medicina di Emergenza Urgenza Pediatrica - Nell’ambito della SIMEUP nazionale è uno degli istruttori di simulazione pediatrica e a tal fine organizza costantemente corsi di formazione presso l’Istituto Gaslini di Genova e da quest’anno ha organizzato una collaborazione con l’Università di Stato di Mosca, per l’aggiornamento dei pediatri attraverso la simulazione, culminato in luglio nella realizzazione del primo convegno Italo-Russo di simulazione nelle Emergenze Pediatriche. - Dal 29 ottobre 2009 al 29 0ttobre 2012 è Consigliere Nazionale SIMEUP. Attività assistenziale Ha creato in clinica Pediatrica un Servizio di Nefrologia, Dialisi e Trapianto Pediatrico che garantisce l’assistenza nefrologica, dialitica e trapiantologica pediatrica. Il servizio è in grado di assicurare trattamenti dialitici dall’età neonatale ( dai prematuri di 600 gr) fino ai bambini in età adolescenziale, con tecniche di dialisi peritoneale, emofiltrazione e emodialisi. E’ il servizio di riferimento pediatrico del centro trapianti della nostra università, con essi ha eseguito: - 62 trapianti pediatrici di cui 54 di rene e 8 di fegato - il primo caso al mondo di trapianto renale in una bambina affetta da acidemia Metilmalonica il primo trapianto pediatrico italiano fegato-rene in un caso di ossalosi - attualmente garantisce la preparazione dei bambini al trapianto, il loro inserimento in lista d’attesa ed il loro follow-up post trapianto sia semiintensivo che ordinario Pubblicazioni Di seguito sono riportati i suoi lavori internazionali più importanti. Lubrano R, Cecchetti C, Elli M, Tomasello C, Guido G, Di Nardo M, Masciangelo R, Pasotti E, Barbieri MA, Bellelli E, Pirozzi N. Prognostic value of extravascular lung water index in critically ill children with acute respiratory failure . Intensive Care Med 2010 Sep 29 (Epub ahead of print) Lubrano R, Versacci P, Guido G, Belleli E, Andreoli G, Elli M. Might there be an association between polycystic kidney desease and noncompaction of the ventricular myocardium. Nephrol Dial Transplant 2009; 24:3884-6. Lubrano R, Travasso E, Raggi C, Guido G, Masciangelo R, Elli M. Blood pressure load, proteinuria and renal function in pre-hypertensive children. Pediatr Nephrol. 2009;24:823-31. Lubrano R, Marandola M, Antonucci A, Tellan G, Elli M, Santulli M, Lauria D, Giuliana G, Delogu G. Hypotensive anesthesia with propofol and remifentanil: protective effect of alpha-tocopherol on renal function. J Clin Anesth. 2008;20:164-9. Corrado Cecchetti, Riccardo Lubrano, Sebastian Cristaldi , Francesca Stoppa, Maria Antonietta Barbieri, Marco Elli, Raffaele Masciangelo, Daniela Perrotta, Elisabetta Travasso, Claudia Raggi, Marco Marano, Nicola Pirozzi. Relathionship between global end diastolic volume and cardiac output in critically ill infants and children. Critical Care Medicine 36; 928-932, 2008 Gaeta A, Nazzari C, Verzaro S, Latte MC, Fabri G, Scateni S, Raggi C, Lubrano R, Mancini C. Early evidence of lymphoproliferative disorder: posttransplant monitoring of Epstein-Barr infection in adult and pediatric patients. New Microbiol. 2006 Oct;29(4):231-41. Lubrano R, Elli M, Rossi M, Travasso E, Raggi C, Barsotti P, Carducci C, Berloco P. Renal transplant in methylmalonic acidemia: could it be the best option? Report on a case at 10 years and review Pediatr Nephrol. 2007,22, 1209-14 Lubrano R, Soscia F, Elli M, Ventriglia F, Raggi C, Travasso E, Scateni S, Di Maio V, Versacci P, Masciangelo R, Romero S. Renal and cardiovascular effects of angiotensin-converting enzyme inhibitor plus angiotensin II receptor antagonist therapy in children with proteinuria. Pediatrics 2006; 118: 833-838 Lubrano R, Romero S, Scoppi P, Cocchi G, Baroncini S, Elli M, Turbacci M, Scateni S, Travasso E, Benedetti R, Cristaldi S, Moscatelli R.How to become an under 11 rescuer: a practical method to teach first aid to primary schoolchildren. Resuscitation. 2005 Mar;64(3):303-7 De Biase A, Ottolenghi L, Polimeni A, Benvenuto A, Lubrano R, Magliocca FM.Bilateral mandibular cysts associated with cyclosporine use: a case report. Pediatr Nephrol. 2001 Dec;16(12):993-5. Lubrano R, Scoppi P, Barsotti P, Travasso E, Scateni S, Cristaldi S, Castello MA..Kidney transplantation in a girl with methylmalonic acidemia and end stage renal failure. Pediatr Nephrol. 2001 Nov;16(11):848-51. Multari G, Werner B, Cervoni M, Lubrano R, Costantino F, Demiraj V, Pozzilli P.Peritoneal dialysis in an infant with type 1 diabetes and hyperosmolar coma. J Endocrinol Invest. 2001 Feb;24(2):104-6. Lubrano R, Meloni C, di Villahermosa SM, Morosetti M, Taccone-Gallucci M.Red blood cell membrane oxidative damage and renal impairment in uremic patients under conservative treatment. Nutrition. 2000 Jan;16(1):86. Taccone-Gallucci M, Meloni C, Lubrano R, Morosetti M, Palombo G, Cianciulli P, Scoppi P, Castello MA, Casciani CU.Chronic haemolysis and erythrocyte survival in haemodialysis patients treated with vitamin Emodified dialysis filters. Contrib Nephrol. 1999;127:44-8. Taccone-Gallucci M, Lubrano R, Meloni C. Vitamin E as an antioxidant agent. Contrib Nephrol. 1999;127:32-43. Gallucci MT, Lubrano R, Meloni C, Morosetti M, Manca di Villahermosa S, Scoppi P, Palombo G, Castello MA, Casciani CU. Red blood cell membrane lipid peroxidation and resistance to erythropoietin therapy in hemodialysis patients. Clin Nephrol. 1999 Oct;52(4):239-45 Taccone-Gallucci M, Lubrano R, Meloni C, Morosetti M, Adolfo CM, Casciani CU.Malonyldialdehyde content of cell membranes is the most important marker of oxidative stress in haemodialysis patients. Nephrol Dial Transplant. 1998 Oct;13(10):2711-2 Castello MA, Ragni G, Antimi A, Todini A, Patti G, Lubrano R, Clerico A, Calisti A.Successful management with interferon alpha-2a after prednisone therapy failure in an infant with a giant cavernous hemangioma. Med Pediatr Oncol. 1997 Mar;28(3):213-5. Berloco P, Pretagostini R, Poli L, Rossi M, Iappelli M, Di Nicuolo A, Venettoni S, De Simone P, Cancrini C, Novelli G, Alfani D, Cortesini R, Lubrano R, Castello MA.Pediatric renal transplantation: personal experience. Transplant Proc. 1996 Feb;28(1):282-3 Taccone-Galluci M, Lubrano R, Trapasso E, Clerico A, Latorre P, Meloni C, Morosetti M, Castello MA, Casciani CU.Oxidative damage to RBC membranes and pentose phosphate shunt activity in hemodialysis patients after suspension of erythropoietin treatment. ASAIO J. 1994 Jul-Sep;40(3):M663-6. Lubrano R, Trapasso E, Brenna S, Castello MA, Pretagostini R, Alfani D, Poli L, Berloco P, Cortesini R.Outcome of kidney function in pediatric transplantation. Transplant Proc. 1994 Feb;26(1):52-3 Pachi A, Lubrano R, Maggi E, Giancotti A, Giampa G, Elli M, Mannarino O, Castello MA.Renal tubular damage in fetuses with intrauterine growth retardation. Fetal Diagn Ther. 1993 Mar-Apr;8(2):109-13 Taccone-Gallucci M, Lubrano R, Clerico A, Meloni C, Morosetti M, Meschini L, Elli M, Trapasso E, Castello MA, Casciani CU.Administration of GSH has no influence on the RBC membrane: oxidative damage to patients on hemodialysis. ASAIO J. 1992 Oct-Dec;38(4):855-857 Lubrano R, Taccone-Gallucci M, Piazza A, Morosetti M, Meloni C, Citti G, Mannarino O, Castello MA, Casciani CU.Vitamin E supplementation and oxidative status of peripheral blood mononuclear cells and lymphocyte subsets in hemodialysis patients. Nutrition. 1992 Mar-Apr;8(2):94-7 Taccone-Gallucci M, Lubrano R, Belli A, Meloni C, Morosetti M, Meschini L, Elli M, Boffo V, Pisani F, Giardini O, et al. Disappearance of oxidative damage to red blood cell membranes in uremic patients following renal transplant. ASAIO Trans. 1989 Jul-Sep;35(3):533-5. Lubrano R, Frediani T, Citti G, Cardi E, Mannarino O, Elli M, Cozzi F, Giardini O.Erythrocyte membrane lipid peroxidation before and after vitamin E supplementation in children with cholestasis. J Pediatr. 1989 Sep;115(3):380-4 Taccone-Gallucci M, Lubrano R, Belli A, Citti G, Morosetti M, Meloni C, Elli M, Mazzarella V, Tozzo C, Meschini L, et al.Lack of oxidative damage in serum polyunsaturated fatty acids before and after dialysis in chronic uremic patients. Int J Artif Organs. 1989 Aug;12(8):515-8. Taccone-Gallucci M, Lubrano R, Del Principe D, Menichelli A, Giordani M, Citti G, Morosetti M, Meloni C, Mazzarella V, Meschini L, et al. Platelet lipid peroxidation in haemodialysis patients: effects of vitamin E supplementation. Nephrol Dial Transplant. 1989;4(11):975-8. Taccone-Gallucci M, Casciani CU, Lubrano R, Giardini O. Vitamin E status in CAPD patients. Nephrol Dial Transplant. 1989;4(1):75-6 Taccone-Gallucci M, Lubrano R, Bandino D, Citti G, Attard-Barbini D, Mazzarella V, Elli M, Meloni C, Morosetti M, Tozzo C, et al.Discrepancies between serum and erythrocyte concentrations of vitamin E in hemodialysis patients: role of HDL-bound fraction of vitamin E. Artif Organs. 1988 Oct;12(5):379-8 Taccone-Gallucci M, Giardini O, Lubrano R, Bandino D, Mazzarella V, Mannarino O, Meloni C, Morosetti M, Elli M, Tozzo C, et al.Red blood cell lipid peroxidation in predialysis chronic renal failure. Clin Nephrol. 1987 May;27(5):238-242 Lubrano R, Taccone-Gallucci M, Mazzarella V, Bandino D, Citti G, Elli M, Giardini O, Casciani CU.Relationship between red blood cell lipid peroxidation, plasma hemoglobin, and red blood cell osmotic resistance before and after vitamin E supplementation in hemodialysis patients. Artif Organs. 1986 Jun;10(3):245-8 Del Principe D, Menichelli A, Lubrano R, Bandino D, Di Giulio S, Di Corpo ML, Giardini O. Vitamin E consumption by human blood platelets activated by latex particles. Am J Hematol. 1986 Apr;21(4):351-6. Taccone-Gallucci M, Giardini O, Ausiello C, Piazza A, Spagnoli GC, Bandino D, Lubrano R, Taggi F, Evangelista B, Monaco P, et al.Vitamin E supplementation in hemodialysis patients: effects on peripheral blood mononuclear cells lipid peroxidation and immune response. Clin Nephrol. 1986 Feb;25(2):81-6. Taccone-Gallucci M, Giardini O, Lubrano R, Mazzarella V, Bandino D, Khashan S, Mannarino O, Elli M, Cozzari M, Buoncristiani U, et al. Red blood cell membrane lipid peroxidation in continuous ambulatory peritoneal dialysis patients. Am J Nephrol. 1986;6(2):92-5. Giardini O, Taccone-Gallucci M, Lubrano R, Ricciardi-Tenore G, Bandino D, Silvi I, Paradisi C, Mannarino O, Citti G, Elli M, et al.Effects of alphatocopherol administration on red blood cell membrane lipid peroxidation in hemodialysis patients. Clin Nephrol. 1984 Mar;21(3):174-7. Giardini O, Pratesi G, Antimi M, Bandino D, Lubrano R, Silvi I, Qaddourah M, Khashan S.Intestinal absorption of tocopherols in homozygous betathalassemia. A study of twenty patients. Haematologica. 1984 Mar-Apr;69(2):127-32 Giardini O, Taccone-Gallucci M, Lubrano R, Ricciardi-Tenore G, Bandino D, Silvi I, Ruberto U, Casciani CU.Evidence of red blood cell membrane lipid peroxidation in haemodialysis patients. Nephron. 1984;36(4):235-7 Raffaele Falsaperla Ho conseguito la Specializzazione in Pediatria ind. Pediatria generale presso l’Università di Catania e il dottorato di Ricerca in Scienze pediatriche discutendo una tesi sulle distrofie muscolari congenite. Grazie agli insegnamenti e al sostegno del Prof. Pavone ho coltivato l’interesse per la diagnosi e il trattamento delle malattie neuromuscolari facendo esperienza di studio presso la Tufts University di Boston con il Prof Munsat e Adelman. Nel 1997 sono entrato con la qualifica di EP presso l’Università di Catania come Dirigente medico di I livello dove ho continuato a collaborare con il Prof. Pavone per la diagnostica bioptica delle patologie neurologiche pediatriche e facendo esperienza nel campo della neurologia e cardiologia pediatrica. Da 3 anni dirigo la UOC di Pediatria con un PSP che drena circa 20.000 accessi/annui e 20 posti letto in regime di degenza ordinaria dove è possibile effettuare la diagnostica neurofisiologica (V-EEG) e bioptica (biopsia muscolare) delle patologie di pertinenza neuropediatrica. FORMATO EUROPEO PER IL CURRICULUM VITAE INFORMAZIONI PERSONALI Nome CF Indirizzo Telefono Fax E-mail Nazionalità Data di nascita FALSAPERLA, RAFFAELE FLSRFL65T29C351S 6/b-6/c, Via Ferrarotto, I - 95125 Catania 095339388 – 3382756653 0957435451 [email protected] Italiana 29 DICEMBRE 1965 ESPERIENZA LAVORATIVA • Date (da – a) • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore • Tipo di impiego • Principali mansioni e responsabilità • Date (da – a) • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore Dal 22 gennaio 2010 Facoltà Scienze della Formazione, Università di Catania Universitaria Docente Insegnamento: Cattedra di Pediatria Preventiva e Sociale Dal 1 aprile 2008 a tutt’oggi Azienda Ospedaliera - Università Vittorio Emanuele – Ferrarotto – S: Bambino, Catania Ospedaliero Universitaria • Tipo di impiego • Principali mansioni e responsabilità Pediatra Direttore struttura complessa UO Pediatria • Date (da – a) • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore • Tipo di impiego • Principali mansioni e responsabilità • Date (da – a) Dal 15 luglio 1997 a 31 marzo 2008 Azienda Ospedaliero Universitaria Policlinico “Gaspare Rodolico”, 78, Via Santa Sofia, I – 95125 Catania Ospedaliero Universitaria Pediatra Dirigente medico I livello Da 1 Ottobre 1996 a 10 Aprile 1997 • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore • Tipo di impiego • Principali mansioni e responsabilità New England Medical Center, Neuropathology directed by Dr. L. Adelman, 800, Washington Street , USA – 02111 Boston (Massachusetts) Ospedaliero Universitaria Fellowship Diagnostica strumentale delle malattie neuromuscolari infantili • Date (da – a) • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore • Tipo di impiego • Principali mansioni e responsabilità Da Gennaio 1995 a giugno 1995 New England Medical Center, Neuromuscular Research directed by Dr. T. Munsat, 800, Washington Street , USA – 02111 Boston (Massachusetts) Ospedaliero Universitaria Fellowship Diagnostica clinica e strumentale delle malattie neuromuscolari infantili (Vedi Allegati 11/a e 11/b) • Date (da – a) • Nome e indirizzo del datore di lavoro • Tipo di azienda o settore • Tipo di impiego • Principali mansioni e responsabilità Da marzo 1992 a maggio 1992 Centro per le malattie neuromuscolari Paolo Peirolo, Ospedale San Giovanni Battista, 15, Via Cherasco, I – Torino Ospedaliero Universitaria Medico in formazione Semeiologia clinica e strumentali delle malattie muscolari infantili ISTRUZIONE E FORMAZIONE • Date (da – a) • Nome e tipo di istituto di istruzione o formazione • Principali materie / abilità professionali oggetto dello studio • Qualifica conseguita Dal 29 Novembre al 4 Dicembre 1999 Università di Messina Iter diagnostico delle malattie neuromuscolari Perfezionamento in Diagnostica Multidisciplinare delle Malattie Neuromuscolari • Livello nella classificazione nazionale (se pertinente) • Date (da – a) • Nome e tipo di istituto di istruzione o formazione • Principali materie / abilità professionali oggetto dello studio • Qualifica conseguita • Livello nella classificazione nazionale (se pertinente) Dal settembre 1995 al maggio 1999 Università degli Studi di Catania Scienze Pediatriche con formazione alla ricerca particolarmente nel campo delle Distrofie Muscolari Congenite Dottorato di ricerca in Scienze Pediatriche X ciclo III livello degli studi universitari • Date (da – a) • Nome e tipo di istituto di istruzione o formazione • Principali materie / abilità professionali oggetto dello studio • Qualifica conseguita • Livello nella classificazione nazionale (se pertinente) Da 1 al 6 Dicembre 1997 Università di Messina • Date (da – a) • Nome e tipo di istituto di istruzione o formazione • Principali materie / abilità professionali oggetto dello studio • Qualifica conseguita • Livello nella classificazione nazionale (se pertinente) Dal settembre 1990 al Luglio 1994 Università di Catania Biopsia Muscolare Perfezionamento in Diagnostica Multidisciplinare delle Malattie Neuromuscolari Scienze Pediatriche con formazione elettiva in neuropediatria Specialista in Pediatria Ind. Pediatria Generale, Voto 50/50 e lode III livello degli studi universitari Marc Berg PERSONAL INFORMATION Date of birth: June 8, 1967 Place of birth: Waconia, Minnesota Present address: 7708 N. Village Ave. Tucson, Arizona 85704 (520) 975-1289 (home) Business address: 1501 N. Campbell Avenue P.O. Box 245073 Tucson, Arizona 85724-5073 (520) 626-5485 (office) (520) 626-6571 (fax) [email protected] EDUCATION 1989 College of Biological Sciences, Biology: B.S. University of Minnesota St. Paul, Minnesota 1993 School of Medicine: M.D. University of Minnesota Minneapolis, Minnesota POSTGRADUATE TRAINING 1993-1994 Pediatric Internship – Department of Pediatrics University of Arizona Health Sciences Center Tucson, Arizona 1994-1996 Pediatric Residency – Department of Pediatrics University of Arizona Health Sciences Center Tucson, Arizona 1996-1997 Chief Resident – Department of Pediatrics University of Arizona Health Sciences Center Tucson, Arizona 1997-2000 Pediatric Critical Care Medicine Fellowship Primary Children’s Medical Center University of Utah Salt Lake City, Utah CERTIFICATION 2002 2002 Pediatric Advanced Life Support (PALS) Instructor, current Human Subjects Protection, Current 2002 Introduction to Animal Hazards, Current 2000 Pediatric Critical Care Medicine, American Board of Pediatrics, current 1999 Advanced Trauma Life Support (ATLS) Provider 1997 General Pediatrics, American Board of Pediatrics, current 1993 Pediatric Advanced Life Support (PALS) Provider, current 1993 Neonatal Resuscitation Program, current LICENSURE 2003 2000 1997 1996 DEA Licensure #BB6746032, current State of Michigan Medical License #4301075650, inactive State of Utah Medical License #344504-1205, inactive State of Arizona Medical License #23628, current MAJOR FIELD(S) OF INTEREST Pediatrics Pediatric Critical Care Resuscitation Science, Pediatric Ventricular Fibrillation and CPR performance Quality and Safety CHRONOLOGY OF EMPLOYMENT 2006-present Associate Professor of Clinical Pediatrics Department of Pediatrics University of Arizona College of Medicine Tucson, Arizona 2003-2009 Medical Director Pediatric Intensive Care Unit Tucson Medical Center Tucson, Arizona 2002-present Associate Staff Department of Pediatrics Tucson Medical Center Tucson, Arizona 2002-present 2002-present 2001-2006 2001-present 2000-2002 Physician and Scientist Sarver Heart Center University of Arizona Tucson, Arizona Pediatric Advanced Life Support Medical Director College of Medicine University of Arizona Tucson, Arizona Assistant Professor of Clinical Pediatrics Department of Pediatrics University of Arizona College of Medicine Tucson, Arizona Affiliate Member in Pediatric Critical Care Children’s Clinics for Rehabilitative Services (CCRS) Tucson, Arizona Assistant Professor of Clinical Pediatrics and Human Development College of Human Medicine Michigan State University East Lansing, Michigan HONORS AND AWARDS 2008 Recognition Award, “Most Up-To-Date Physician” presented by Tucson Medical Center, Tucson Arizona 2007 Awarded the L. Barry Seltz Memorial Award for “Excellence in Teaching” by the Arizona Health Sciences Center Graduating Class of 2007, University of Arizona, Tucson, Arizona. 2007 Awarded the Off Service Attending Award for “Dedication and Excellence in Teaching”, by the Arizona Health Sciences Center Emergency Medicine Graduating Class of 2007, University of Arizona, Tucson, Arizona. 2004 Awarded the Off Service Attending Award for “Dedication and Excellence in Teaching”, by the Arizona Health Sciences Center Emergency Medicine Graduating Class of 2004, University of Arizona, Tucson, Arizona. 2003 Awarded the Off Service Attending Award for “Dedication and Excellence in Teaching”, by the Arizona Health Sciences Center Emergency Medicine Graduating Class of 2003, University of Arizona, Tucson, Arizona. 2002 Nominated for the Vernon and Virginia Furrow award for “Excellence in Innovation in Teaching.” 1997 Awarded “Excellence in Medical Student Teaching by a Houseofficer”, by the School of Medicine, University of Arizona, Tucson, Arizona. 1996 Awarded the “Pediatric Resident Excellence in Research”, by the Department of Pediatrics, University of Arizona, Tucson, Arizona. COMMITTEES 2011 – Present Member, UA Healthcare Governance Council 2010 – Present Member, UA Healthcare CEO Search Committee 2010 – Present Member, University Physicians Healthcare Corporate Compliance Committee 2009 – Present Member, University Physicians Healthcare/University Medical Center Board of Directors, ad hoc Committee on Merger 2009 – Present Chairman, UPH Board of Directors Quality Committee 2009 – Present Chairman, American Heart Association (AHA) Emergency Cardiac Care, (ECC), Pediatric Sub-committee (PALS) 2008 – Present Director, University Physicians Healthcare (UPH) Board of Directors 2008 – Present Clinical Investigator, Venom Immunochemistry, Pharmacology, and Emergency Response (VIPER) Institute 2007 - 2009 Chairman-elect, American Heart Association (AHA) Emergency Cardiac Care (ECC), Pediatric Sub-committee (PALS) 2007 - 2010 Chairman University Physicians Healthcare Practice Compliance and Ethics Committee, Tucson, Arizona. 2006 – 2007 Member, University Physicians Healthcare Practice Compliance and Ethics Committee, Tucson, Arizona. 2006 - Present Member, Medical Simulation Committee, Arizona Health Sciences Center 2005 - 2007 Member, Steering Committee,100,000 Lives Campaign Initiative in Patient Care and Safety Improvement, University Medical Center. Tucson, Arizona. 2005 - Present Chairman Rapid Response Team (RRT) Committee, University Medical Center. Tucson, Arizona. 2004 - 2007 Young scientist Member, American Heart Association (AHA) Emergency Cardiac Care (ECC), Pediatric Sub-committee (PALS) 2005 - 2007 Invited member as young scientist to the International Liaison Committee on Resuscitation (ILCOR) 2002 - Present Resident Education Committee of the Pediatric Section of the Society of Critical Care Medicine 2003 - Present Education Committee, Department of Pediatrics, University of Arizona. Tucson, Arizona 2003 - 2009 Committee to Organize Improved Community Physician Relations 2002 - 2009 Pediatric Clinical Practice Team Committee, Tucson Medical Center. Tucson, Arizona 2002 - 2006 Pediatric Strategy Committee, Tucson Medical Center. Tucson, Arizona 2002 - 2009 Department of Emergency Medicine Peer-review committee, Tucson Medical Center. Tucson, Arizona 1996 - 1997 Pediatric Asthma Management Protocol Task Force, School of Medicine, University of Arizona. Tucson, Arizona 1996 - 1997 Pediatric Service Team Committee, School of Medicine, University of Arizona. Tucson, Arizona 1996 – 1997 Pediatric Advisory Committee, Tucson Medical Center Tucson, Arizona 1996 - 2008 Pediatric Chart Review Committee, Tucson Medical Center Tucson, Arizona 1995 – 1997 Pediatric Housestaff Committee, School of Medicine, University of Arizona. Tucson, Arizona 1995 – 1997 Pediatric Resident Admissions Committee, School of Medicine, PROFESSIONAL ORGANIZATIONS 2008 – Present 1998 - Present 1993 - Present 1989 – 1993 1990 -- 1991 Member of American Heart Association 2002 - PresentPima County Pediatric Society Society of Critical Care Medicine, Candidate Fellow American Academy of Pediatrics, Fellow American Medical Student Association Vice-President, American Medical Student Association (AMSA), University of Minnesota - Duluth Chapter. PROFESSIONAL SERVICE 2006 - 2007 Preceptor/Mentor for Introduction to Clinical Medicine, University of Arizona, College of Medicine. Tucson, Arizona. 2006 - 2007 Course Director Pediatric Enrichment Elective, University of Arizona, College of Medicine 2005 - 2006 Preceptor/Mentor for Introduction to Clinical Medicine, University of Arizona College of Medicine, Tucson, Arizona. 2005 - Present Established Framework of and System for Coordinated Hospital-wide Medical Emergency Team (MET) and Rapid Response Team (RRT), UMC, Tucson, Arizona. 2005 - Present Course director Pediatric Enrichment Elective, University of Arizona College of Medicine. 2004 - Present Volunteer, American Heart Association, Pediatric Advanced Life Support (PALS) course 2003 - Present Manuscript and Peer Reviewer for Pediatrics and Acta Pediatrica and Critical Care Medicine and Pediatric Critical Care Medicine. 10-11/2003 Department Faculty Representative for Residency Review Committee site visit. 2002 - Present Course director Pediatric Advanced Life Support, University of Arizona, Tucson, Arizona. 2002 - 2005 Instructor for University of Arizona 1st and 2nd year Medical Students in the Pediatric Enrichment Elective. 2002 Prepared Induced Hypothermia Protocol for University Medical Center, Tucson, Arizona. 2001 Questions Writer for the American Board of Pediatrics-Pediatric Critical Care Medicine Board Examination. 03/1999 Team Physician and Pediatric Intensivist for Operation Smile mission to Yasathon, Thailand. PUBLICATIONS/CREATIVE ACTIVITY Book Chapters: 1. Berg MD, Nadkarni VM, Gausche-Hill M, Kaji AH, Berg RA. “Pediatric Resuscitation.” Rosen’s Emergency Medicine Concepts and Clinical Practice 7th Edition. ed: Marx JA, Hockberger RS, Walls RM. Mosby Elsevier. Philadelphia, PA. 2010. 64:76. 2. Berg MD, Meyer RJ. ”Gas Exchange, Oxygen Delivery, and Ventilation.” Pediatric Respiratory Medicine 2nd Edition. ed: Taussig LM, Landau LI. Mosby Elsevier. Philadelphia, PA. 2008. 179:200 Refereed Journal Articles: 1. Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, Berg MD, Chameides L, O'Connor RE, Swor RA. Part 4: CPR Overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S676-S684. 2. Link MS, Atkins DL, Passman RS, Halperin HR, Samson RA, White RD, Cudnik MT, Berg MD, Kudenchuk PJ, Kerber RE. Part 6: Electrical Therapies: Automated External Defibrillators, Defibrillation, Cardioversion and Pacing • 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S706-S719. 3. Berg MD, Schexnayder SM, Chameides L, Terry M, Donoghue A, Hickey RW, Berg RA, Sutton RM, Hazinski MF. Part 13: Pediatric Basic Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S862-S875. 4. Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL, Berg MD, de Caen AR, Fink EL, Freid EB, Hickey RW, Marino BS, Nadkarni VM, Proctor LT, Qureshi FA, Sartorelli K, Topjian A, van der Jagt EA, Zaritsky AL. Part 14: Pediatric Advanced Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S876-S908. 5. Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk P , Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, MS, Morrison LJ, O'Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD,Vanden Hoek, TL. Part 1: Executive Summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640-S656. Link 6. Zuercher M, Hilwig RW, Ranger-Moore J, Nysaether J, Nadkarni VM, Berg MD, Kern KB, Sutton R, Berg RA. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Critical Care Medicine. 2010 Apr;38(4):1141-1146. 7. Indik JH, Hilwig RW, Zuercher M, Kern KB, Berg MD, Berg RA. Preshock cardiopulmonary resuscitation worsens outcome from circulatory phase ventricular fibrillation with acute coronary artery obstruction in swine. Circulation: Arrhythmia and Electrophysiology. 2009 Apr;2(2):179-84. 8. Berg MD. Pediatric in-hospital cardiac arrest and therapeutic hypothermia: where we are and where we are going. Pediatric Critical Care Medicine. 2009 Sep;10(5):601-2. 9. Berg MD, Nadkarni VM, Berg RA. CPR-why the new emphasis? Pediatric Clinics of North America. 2008 Aug;55(4):861-72. 10. Indik JH, Donnerstein RL, Hilwig RW, Zuercher M, Feigelman J, Kern KB, Berg MD, Berg RA. The influence of myocardial substrate on ventricular fibrillation waveform: a swine model of acute and postmyocardial infarction. Critical Care Medicine. 2008;36(7):2136-42. 11. Berg MD, Nadkarni VM, Zuercher M, Berg RA. In-hospital pediatric cardiac arrest. Pediatric Clinics of North America. 2008 Jun;55(3):589-604. 12. Berg MD, Banville IL, Chapman FW, Walker RG, Gaballa MA, Hilwig RW, Samson RA, Kern KB, Berg RA. Attenuating the defibrillation dosage decreases postresuscitation myocardial dysfunction in a swine model of pediatric ventricular fibrillation. Pediatric CriticalCare Medicine. 2008 Jul;9(4):42934. 13. Berg RA, Hilwig RW, Berg MD, Berg DD, Samson RA, Indik JH, Kern KB. Immediate post-shock chest compressions improve outcome from prolonged ventricular fibrillation. Resuscitation. 2008 Jul;78(1):71-6. 14. Berg MD, Nadkarni VM, Berg RA. Cardiopulmonary resuscitation in children. Current Opinion Critical Care. 2008 Jun;14(3):254-60. 15. Indik JH, Donnerstein RL, Berg RA, Hilwig RW, Berg MD, Kern KB. Ventricular fibrillation frequency characteristics are altered in acute myocardial infarction. Critical Care Medicine. 2007 Apr;35(4):1133-8. 16. Samson RA, Nadkarni VM, Meaney PA, Carey SM, Berg MD, Berg RA; American Heart Association National Registry of CPR Investigators. Outcomes of in-hospital ventricular fibrillation in children. N Engl J Med. 2006 Jun 1;354(22):2328-39. 17. Samson RA, Berg MD, Berg RA. Cardiopulmonary resuscitation algorithms, defibrillation and optimized ventilation during resuscitation. Current Opinion Anesthesiology. 2006 Apr;19(2):146-56. 18. Berg MD, Samson RA, Meyer RJ, Clark LL, Valenzuela TD, Berg RA. Pediatric defibrillation doses often fail to terminate prolonged out-of-hospital ventricular fibrillation in children. Resuscitation. 2005 Oct;67(1):63-7. 19. Valenzuela TD, Kern KB, Clark LL, Berg RA, Berg MD, Berg DD, Hilwig RW, Otto CW, Newburn D, Ewy GA. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation. 2005 Aug 30;112(9):1259-65. 20. Berg RA, Samson RA, Berg MD, Chapman FW, Hilwig RW, Banville I, Walker RG, Nova RC, Anavy N, Kern KB. Better outcome after pediatric defibrillation dosage than adult dosage in a swine model of pediatric ventricular fibrillation. Journal of the American College of Cardiology. 2005 Mar 1;45(5):786-9. 21. Berg MD, Clark LL, Valenzuela TD, Kern KB, Berg RA. Post-shock chest compression delays with automated external defibrillator use. Resuscitation. 2005 Mar;64(3):287-91. 22. Kern KB, Valenzuela TD, Clark LL, Berg RA, Hilwig RW, Berg MD, Otto CW, Newburn D, Ewy GA. An alternative approach to advancing resuscitation science. Resuscitation. 2005 Mar;64(3):261-8. Review. 23. Indik JH, Donnerstein RL, Berg MD, Samson RA, Berg RA. Ventricular fibrillation frequency characteristics and time evolution in piglets: a developmental study. Resuscitation. 2004 Oct;63(1):85-92. 24. Berg RA, Chapman FW, Berg MD, Hilwig RW, Banville I, Walker RG, Nova RC, Sherrill D, Kern KB. Attenuated adult biphasic shocks versus weight-based monophasic shocks in a swine model of prolonged pediatric ventricular fibrillation. Resuscitation. 2004 May; 61: 189-197. 25. Berg MD, Cook L, Cornelia HM, Vernon DD, Dean JM. Effect of seating position and restraint use on injuries to children in motor vehicle crashes. Pediatrics. 2000 Apr;105(4 Pt 1): 831-5. 26. Berg MD, Pribble CG. Pneumothorax as a complication of bilevel positive airway pressure (BiPAP) ventilation. Clinical intensive Care. 2000; 11(3):145-7. 27. Berg MD, Idris AH, Berg RA. Severe ventilatory compromise due to gastric distention during pediatric cardiopulmonary resuscitation. Resuscitation. 1998 Jan; 36(1):71-3. 28. Berg RA, Kern KB, Hilwig RW, Berg MD, Sanders AB, Otto CW, Ewy GA. Assisted Ventilation does not improve outcome in a porcine model of single-rescuer bystander cardiopulmonary resuscitation. Circulation. 1997 Mar 18; 95(6):1635-41. Abstracts: 1. Julia H. Indik, M.D., Ph.D; Richard L. Donnerstein, M.D.; Ronald W. Hilwig, D.V.M., Ph.D.; Mathias Zuercher, M.D.; Justin Feigelman, B.A.; Karl B. Kern, M.D.; Marc D. Berg, M.D.; Robert A. Berg, M.D.: The Influence of Myocardial Substrate upon Ventricular Fibrillation Waveform: A swine Model of Acute and Post-Myocardial Infarction. 2008 2. Peter A. Meaney; Vinay Nadkami; Ricardo Samson; Marc Berg; G L Larkin; Berg Robert: The Importance of Illness Category on Initial Cardiac Arrest Rhythm and Defibrillation Outcome in the National Registry for Cardiopulmonary Resuscitation: 242-S. Critical Care Medicine. Society of Critical Care Medicine 35th Critical Care Congress San Francisco, Califormia, USA January 7–11, 2006. 33(12) Abstract Supplement A67, December 2005. 3. Peter A. Meaney; Vinay Nadkami; Ricardo Samson; Scott Carey; Marc Berg; Berg Robert: Pediatric In-Hospital Ventricular Fibrillation: Results From the National Registry for Cardiopulmonary Resuscitation: 241-S. Critical Care Medicine. Society of Critical Care Medicine 35th Critical Care Congress San Francisco, California. USA January 7–11, 2006. 33(12) Abstract Supplement A67, December 2005. 4. Marc D Berg, University of Arizona, Tucson, Arizona; Isabelle L Banville, Fred W Chapman, Medtronic ERS, Redmond, WA; Ronald W Hilwig, University of Arizona, Tucson, Arizona; Robert G Walker, Medtronic, Redmond, WA; Richard C Nova, Medtronic ERS, Redmond, WA; Karl B Kern, Robert A Berg, University of Arizona, Tucson, Arizona. Evaluation of a New, Lower Dose for Pediatric Defibrillation with Automated External Defibrillators. Presented at the University of Arizona, Tucson, Arizona. 5. Julia Indik, Richard L Donnerstein, Robert A Berg, Ronald W Hilwig, Marc D Berg, Karl B Kern. Ventricular Fibrillation Frequency Characteristics are Altered in Acute Myocardial Infarction. Presented at the Sarver Heart Center, Tucson, Arizona. 6. Berg MD, Samson RA, Donnerstein RL, Clark L, Indik JH, Neibler R, Berg D, Kern KB, Berg RA. P-Waves During Ventricular Fibrillation (VF) May Result in Malfunction of an Automated External Defibrillator (AED). Presented at the American Heart Association Resuscitation Science Symposium (Dallas, TX), Best Original Resuscitation Science. November 11-12, 2005 7. Valenzuela TD, Indik JH, Kern KB, Clark L, Berg RA, Berg MD, Berg D, Hilwig RW, Otto CW, Newburn D, Ewy GA. Interruption of Chest Compressions During Emergency Medical Systems Resuscitation. Presented at the American Heart Association Resuscitation Science Symposium (Dallas, TX), Best Original Resuscitation Science. November 11-12, 2005. 8. Berg RA, Hilwig RW, Berg MD, Indik JH, Kern KB. Prompt Post-shock Chest Compressions Improve Outcome from Prolonged Ventricular Fibrillation. Presented at the American Heart Association Resuscitation Science Symposium (Dallas, TX), November 11-12, 2005. 9. Berg RA, Chapman FW, Berg MD, Hilwig, RW, Banville I, Walker RB, Kern KB. Attenuated vs Adult Biphasic Shocks in a Swine Model of Prolonged Pediatric Ventricular Fibrillation. Presented at the International Interdisciplinary Conference on Emergencies (IICE) (Montreal, Canada), June 26-30, 2005. 10. Berg MD, Samson RA, Meyer RJ, Clark LL, Valenzuela TD, Berg RA. Pediatric Defibrillation Doses: Less effective in Prolonged Out-Of-Hospital Pediatric Cardiac Arrest. Circulation 2004 110(17): iii-453. Presented at the American Heart Association Scientific Sessions (New Orleans, LA), Clinical Advances in Resuscitation. November 7-10, 2004. 11. Berg RA, Chapman FW, Berg MD, Hilwig RW, Banville I, Walker RG, Nova RC, Kern KB. Defibrillation of pediatric prolonged VF: adult or attenuated dose? Presented at Cardiostim (Nice, France), June 16, 2004. 12. Berg R, Berg MD, Hilwig R, Kern K, Hayes M. Post-shock chest compressions without assisted ventilation improves outcome in a swine model of pre-hospital VF cardiac arrest. Critical Care Medicine 2003; 31:A33. Presented at the 33rd Critical Care Congress (Orlando, FL), February 20-25, 2004. 13. Berg R, Berg MD, Hilwig R, Kern K, Hayes M. One minute or three minutes of prompt uninterrupted post-shock chest compressions are similarly effective for prolonged VF. Critical Care Medicine 2003; 31:A34. Presented at the 33rd Critical Care Congress (Orlando, FL), February 20-25, 2004. 14. Berg MD, Hilwig R, Kern K, Hayes M, Berg R. AED-Delivered stacked shocks versus single shocks in a swine model of pre-hospital VF cardiac arrest. Critical Care Medicine 2003; 31:A33. Presented at the 33rd Critical Care Congress (Orlando, FL), February 20-25, 2004. 15. Berg RA, Chapman FW, Berg MD, Hilwig RW, Banville I, Walker RG, Nova RC, Kern KB. Attenuated adult biphasic shocks versus weight-based monophasic shocks in a swine model of prolonged pediatric ventricular fibrillation. Presented at NAEMSP, January 8, 2004. 16. Berg RA, Hilwig RW, Kern KB, Berg MD, Ewy GA. Piglet biphasic defibrillation with the same dosage over a wide weight range is as safe as monophasic weight-based dosing. Critical Care Medicine 2003; 31:A3. Presented at the 32nd Critical Care Congress, January 28-February 2, 2003. 17. Berg RA, Chapman FW, Berg MD, Hilwig RW, Banville I, Walker RG, Nova RC, Kern KB. Relation Between Defibrillation Dosage and Outcome in a Swine Model of Pediatric Ventricular Fibrillation. Circulation 2003 108(17) Supplement IV: 1030. Presented at the American Heart Association Scientific Sessions (Orlando, FL), November 9-12, 2003. 18. Berg MD, Valenzuela TD, Clark LL, Berg RA. Post-countershock Chest Compression Delays with Automated External Defibrillator Usage. Circulation 2003 108(17) Supplement IV: 2650. Presented at the American Heart Association Scientific Sessions (Orlando, FL), Resuscitation Science: New Vistas and New Controversies. November 9-12, 2003. 19. Berg MD, Valenzuela TD, Clark LL, Berg RA. Delay in the provision of chest compressions with the use of an automatic external defibrillator by emergency medical services personnel after outof-hospital cardiac arrest. Annals of Emergency Medicine. 2002 Oct, Pt 2; 40(4):119. Presented at ACEP (Seattle, WA), September 2002. 20. Berg MD, Cvijanovich N, Maloney C, Moon A, Price M. Use of nasal continuous positive airway pressure (nCPAP) in infants with RSV bronchiolitis. Presented at the World Congress of Pediatric Critical Care (Montreal, Canada), July 2002. 21. Berg MD, Mullett CJ, Allen EA. An internet-based ABG interpretation tutorial is an effective teaching tool for medical students. Clinical Intensive Care 1999 Aug; 10(4):152. Presented at the 12th Annual Pediatric Critical Care Colloquium, Portland, Oregon. September, 1999. 22. Berg MD, Berg RA, Hilwig RW, Kern KB, Sanders, AB, Otto CW, Ewy GA. Assisted ventilation during “bystander” CPR does not improve outcome. Circulation 1995 Oct; 92: I-761. Presented at the 8th Annual Arizona Cardiovascular & Stroke Update, Tucson, Arizona. May 9-10, 1997. 23. Berg RA, Hilwig RW, Kern KB, Berg MD, Sanders, AB, Otto CW, Ewy GA. Assisted ventilation during “bystander” CPR does not improve outcome. Circulation 1995 Oct; 92: I-761. Presented th at the American Heart Association’s 68 Scientific Sessions, Anaheim, California. November 1316, 1995. MEDIA Television: 1. Interview with KVOA-TV, Tucson, Arizona for Pediatric CPR and Drowning. April, 2010 2. Interview with KOLD-TV, Tucson, Arizona for Impacts and Outcomes from Near-Drowning. 3. Interview with UPN 18, Tucson, Arizona for the Children’s Miracle Network at TMC, June 5, 2005. 4. Interview with KGUN-TV, Tucson, Arizona for the Grand Re-opening of the Pediatric Intensive Care Unit at Tucson Medical Center, 2004. Radio: 1. Interview with 93.7 KRQ, Tucson Arizona for Children’s Miracle Network fundraising for Tucson Medical Center. July 2004. 2. Annual Childrens Miracle Network Radio-telethon fundraising for Tucson Medical Center. February 2003. Newspaper: 1. "US Physician Lectures on Importance of Pediatric CPR" Hokkoku Shimbun, June 5, 2010. 2. “TMC Opens 3.9M Pediatrics ICU.” Interview for the Tucson Citizen, August 18, 2004. 3. “Gorgeous “ICU for Kids at TMC.” Interview for the Arizona Daily Star, August 17, 2004. PROGRAM DEVELOPMENT Past Program Development: N/A Present Program Development: Established, host and produced series of ‘Podcasts’ for University Medical Center to inform medical staff of progress in the “Institute for Healthcare Initiatives 100K lives Campaign”. July, 2006. SCHOLARLY PRESENTATIONS 12/2010 12/2010 Invited Lecture: “Paediatric Life Support”, Centro de Congressose Exposições da Alfandega, Porto, Portugal Invited Lecture: “Paediatric BLS”, Centro de Congressos e Exposições da Alfandega, Porto, Portugal 12/2010 Invited Lecture: “Pediatric Advanced Life Support. Do We Need a Change of Training Methods?” Centro Social Caixanova, Plaza De Cervantes, Santiago de Compostela, Spain. 10/2010 Presented: “Pulmonary Physiology and Mechanical Ventilation: Making the Connection.” Pediatric Critical Care Nursing, San Diego, California. 10/2010 Presented: “More on the New Pediatric Basic and Advanced Life Support Guidelines.” Pediatric Critical Care Nursing, San Diego, California. 10/2010 Invited Lecture: “The Physiology of CPR: How Does It Work?” Presented at American Academy of Pediatrics National Conference and Exhibition, San Francisco, California 10/2010 Invited Lecture: “Ventilation and CPR: Do We Go Straight to “C”?” Presented at American Academy of Pediatrics National Conference and Exhibition, San Francisco, California 6/2010 Presentation of “Pediatric Defibrillation: What is the Correct Dose. Presented at 13th Asian-Australasian Congress of Anesthesiologists Fukuoka, Japan 6/2010 Invited Lecture, “Update in Pediatric CPR and Resuscitation: The Science Behind the Controversy” Kanazawa Medical University, Kanazawa Japan 3/2010 Presentation of “Pediatric BLS and ALS Resuscitation: Proposed Changes to the Current Guidelines and the Science Behind Them” to the American Heart Association’s “Stakeholder’s Meeting”, Dallas, TX 1/2010 Invited Lectures, “Pathophhsiology and Categorization of Shock States in Pediatrics” and “Pharmacotherapy for Shock in Children: One Size Does Not Fit All” to the Jornadas de Medicos Residentes de Pediatria Congress of the Hospital Infantil de Mexico Federico Gomez y Instituto Nacional de Pediatria (Federico Gomez Children’s Hospital and National Institute of Pediatrics) Mexico City, Mexico 6/2009 Invited Lecture, “Chest Compresion during CPR: When and How Much?” to the tenth Wolf Creek International Conference on Cardiopulmonary Resuscitation, Indian Wells, CA. 5/2008 Presentation of Current Science Update Pediatric Advanced Life Support (PALS) and presentation on the Grand Opening of the Japan ACLS (JAA) Training Center – Tokyo, Japan 5/2008 Presented, “Interdisciplinary Teaching to Improve Teaching, Quality of Care and Financial Performance” at 2008 AAP 25th Annual Education Meeting, Tucson Arizona. 2/2008 Conference on Pediatric Congenital Heart disease, conducted simulations on “Emergencies in the Cardiac ICU” with the Children’s Hospital of Philadelphia (CHOP) – Scottsdale, AZ 11/2007 Presentation of Pediatric Advanced Life Support (PALS) and introduction of Pediatric Emergency Assessment and Treatment (PEARS) courses – Tokyo University, Tokyo, Japan 6/2007 Invited Lecture, “Rescuer Learning During CPR: Does 10% or 20% Make a Difference?” To the ninth Wolf Creek International Conference on Cardiopulmonary Resuscitation, Indian Wells, CA. 11/2006 Invited Lecturer, “Low dose defibrillation for pediatric ventricular fibrillation” ED Nursing Education Conference. Arizona Health Science Center, Tucson, Arizona. 11/2006 Presented “Pediatric Defibrillation by Attenuating the Adult Dose: How Safe and Effective is it at Low Energy?” at 2006 AHA Scientific Session, November 12-15, Chicago, IL. 10/2006 Invited Lecturer/Instructor, Pediatric Advanced Life Support. American Heart Association Affiliate, Hong Kong, S.A.R., China. 3/2006 Invited Lecturer, “What’s New in CPR”, Sierra Vista Regional Health Center and RW Bliss Army Health Center 9/2005 Invited Lecturer, “What’s New in CPR”, Wilcox Arizona Hospital staff. 6/2005 Invited Lecturer, “What’s New in CPR”, Sierra Vista Regional Health Center and the Benson Hospital staff. 4/2005 Invited Lecturer, “Continuous Chest Compressions CPR, the Science and the Practice,” University of Arizona, Department of Pediatrics staff. 3/2004 Invited Lecturer, “Life Threatening Events in Infancy,” Tucson Hospital Medical Education Programs, Inc., Sierra Vista Regional Health Center, Sierra Vista, Arizona. 3/2004 Invited Lecturer, “New CPR Research and Protocols,” Safety Supervisor’s Meeting, City of Tucson, Tucson, Arizona. 2/2004 Invited Lecturer, “The New CPR,” Healthy Heart, University Medical Center, Tucson, Arizona. 1/2004 Invited Lecturer, “Apparent Life Threatening Events,” Pre-hospital Tape and Chart session, University Medical Center, Tucson, Arizona. 9/2003 Conference, “Multiple Trauma in Pediatrics”, Tucson Medical Center. 9/2003 Conference, “Multiple Trauma in Pediatrics”, Tucson Medical Center. 9/2003 Conference, “Multiple Trauma in Pediatrics”, Tucson Medical Center. 9/2003 Conference, “Care of the Post-Op Orthopedics”, Tucson Medical Center 9/2003 Invited Lecturer, “New initiatives in the treatment of pre-hospital ventricular fibrillation cardiac arrest,” Tucson Fire Department, Public Safety Academy, Tucson, Arizona. 1/2003 Conference, “Latest Update on Monitoring Blood Pressure in Acutely Ill Children”, Tucson Medical Center, Department of Emergency Medicine. 1/2003 Conference, “Latest Update on Monitoring Blood Pressure in Acutely Ill Children”, Tucson Medical Center, Department of Emergency Medicine. 1/2003 Conference, “Latest Update on Monitoring Blood Pressure in Acutely Ill Children”, Tucson Medical Center, Department of Emergency Medicine. 1/2003 Invited Lecturer, “Apparent life threatening events,” Pre-hospital Grand Rounds, University Medical Center, Tucson, Arizona. 10/2002 Invited Lecturer, “Keys to residency success,” University of Arizona College of Medicine, Tucson, Arizona. 10/2002 Research forum educational program-EMS Resuscitation. Berg MD, Valenzuela TD, Clark LL, Berg RA. Delay in the provision of chest compressions with the use of an automatic external defibrillator by emergency medical services personnel after out-of-hospital cardiac arrest. Washington State Convention and Trade Center, Seattle, Washington. 9/2002 Invited Lecturer, “Keys to residency success,” University of Arizona College of Medicine, Tucson, Arizona. 8/2002 Invited Lecturer, “Ask the expert,” Department of Emergency Medicine, University of Arizona Health Sciences Center, Tucson, Arizona. 8/2002 Invited Lecturer, “Keys to residency success,” University of Arizona College of Medicine, Tucson, Arizona. 7/2002 Nursing Education, “Shock, Respiratory Failure and DIC,” Tucson Medical Center, Tucson, Arizona. 08/2000 Resident Lecture Series, “Fluid and electrolyte management in the PICU,” DeVos Children’s Hospital, Grand Rapids, Michigan. 08/2000 Resident Lecture Series, “Running effective codes” and “Orientation to the code cart” DeVos Children’s Hospital, Grand Rapids, Michigan. 1999/2000 Monthly PICU Resident Lecture Series, “Congenital Heart Diseases in Children,” Primary Children’s Medical Center, University of Utah, Salt Lake City, Utah. 5/1999 Emergency Medical Services for Children (EMSC) EMT Training Conference, “Pediatric Trauma and Medical Emergencies,” Cedar Breaks Lodge, Brian Head, Utah. 5/1999 Invited Lecturer, Advanced Neurologic Nursing Course. “SIADH, Diabetes Insipidus and Cerebral Salt Wasting,” Primary Children’s Medical Center, University of Utah, Salt Lake City, Utah. 1/1999 Invited Lecturer, Morning Report. “Chest tubes for the complete pediatrician: Indications, placement and management,” Primary Children’s Hospital, University of Utah, Salt Lake City, Utah. 1998-1999 Monthly PICU Resident Lecture Series. “Recognizing respiratory failure and understanding mechanical ventilation,” Primary Children’s Hospital, University of Utah, Salt Lake City, Utah. 10/1998 Advanced Cardiovascular Nursing Course. “Vasoactive medications in the PICU,” Primary Children’s Hospital, University of Utah, Salt Lake City, Utah. 10/1997 Advanced Cardiovascular Nursing Course. “Vasoactive medications in the PICU,” Primary Children’s Hospital, University of Utah, Salt Lake City, Utah. 6/1996 Department of Pediatrics Conference. “Hypothermia: Diagnosis, pathophysiology and management,” University of Arizona Health Sciences Center, Tucson, Arizona. 5/1996 Pediatric/Emergency Medicine Joint Conference. “Diagnosis and initial stabilization of the child with late-onset Group B streptococcus infection,” University of Arizona Health Sciences Center, Tucson, Arizona. 11/1995 Department of Pediatrics Conference. “Post-streptococcal glomerular nephritis presenting as hemoptysis in an adolescent boy,” University of Arizona Health Sciences Center, Tucson, Arizona. 3/1995 Department of Pediatrics Conference. “Inflammatory pseudotumor in childhood,” University of Arizona Health Sciences Center, Tucson, Arizona. RESEARCH 2011-Present 2010-Present Pending UA site PI for Pharmacologic Impact on Sedation Assessments (PISA) 4 year study UA site PI for Randomized Evaluation of Sedation Titration for Respiratory Failure (RESTORE) 5 Year study UA site PI for Genetic Variations and Biomarkers in Children with Acute Lung Injury (BALI) Pending Allan De Caen PERSONAL INFORMATION Name: Dr. Allan Roland Balleine de Caen Hospital Address: 3A3.06 Walter Mackenzie Health Sciences Center 8440 – 112 Street Edmonton, AB T6G 2B7 Hospital Phone: E-mail: (780) 407-1673 Fax (780) 407-3214 [email protected] CURRENT POSITION Academic appointment Clinical Associate Professor Department of Pediatrics, Faculty of Medicine, University of Alberta (Appointed 2000) Clinical Appointment Pediatric Intensivist Pediatric Intensive Care Transport Physician PICU, Stollery Children’s Hospital, Edmonton 1994-present Administrative duties Alberta Health Services/ CHA Date Committee or responsibility Description of role 1995-present Pediatric Intensive Care Transport Team Stollery Children’s Hospital, Edmonton Pediatric Intensive Care Transport Subcommittee, Pediatric Critical Care Section Child Health Council, Capital Health Authority Regional Trauma Program Committee Capital Health Authority Medical Director 1996- present 1997- 2003 1994- 1996 Co-chair Member 1995- 1997 Morbidity and Mortality Committee, Pediatric Chair Critical Care Section, Child Health Council, Capital Health Authority Pediatric Code Committee, Pediatric Critical Care Chair Section, Child Health Council, Capital Health Authority Trauma Council, Capital Health Authority Member 1994-1996 H.O.P.E. Committee, University of Alberta Hospital 1994- 1996 Member University of Alberta: Department of Pediatrics Date Committee or responsibility Description of role 2005- present Pediatric Critical Care Medicine Residency Program Director Program, 2005- present Pediatric CCM Residency Program Selection Subcom Pediatric Critical Care Medicine Residency Program Com. Pediatric Subspecialty Residency Program Director Com. Pediatric Subspecialty Residency Program Director Com. Post Graduate Pediatric Medical Education Committee General Pediatrics Residency Program Chair Chair 1995- 2005 1997- 2002 General Pediatrics Residency CARMS Selection Comm Medical Education Committee, Dept Pediatrics Pediatric Residency Training Committee Nursing 498 (Pediatric Transport course) 1997-1998 General Pediatrics Residency Program Acting Director 1995-2005 General Pediatrics Residency CARMS Member, file reviewer Selection Comm. General Pediatrics Residency CARMS Member Interview Comm. PICU Rotational coordinator for rotating residents (EM, Pediatrics, Anesthesia, Surgery) 2001-2005 2001- present 2001- 2005 2001- 2005 2001- 2005 2001-2005 2001-2005 1995-2007 1995-2002 Member Member Chair Director Program Director Member and Chair Member Course(s) Director University of Alberta: Faculty Date Committee or Description of role responsibility 2002- present 2001- present Internal Reviews Member Subcommittee, Faculty Post Graduate Medical Education Committee Faculty Post Graduate Medical Member Education Committee Provincial Committees Date Committee or responsibility Description of role 2008-present Board of Directors, Heart and Stroke Foundation of Alberta Research Medical Advisory Committee, Heart and Stroke Foundation of Alberta Resuscitation Committee, Heart and Stroke Association of Alberta Provincial Advanced Life Support Committee, Heart and Stroke Association of Alberta Provincial Advanced Life Support Committee, Heart and Stroke Association of Alberta Director 2010- present 2006- present 2006- present 1998- present Member Vice Chair Chair Member National/ International Committees Date Committee or responsibility Description of role Fall 2010 Chair elect 2006 to present Pediatric subcommittee, American Heart Association Emergency Cardiac Care Committee CAPHC Pediatric National Transportation Systems Systems Design Working Group CAPHC Pediatric National Transportation Systems Committee RCPSC Accreditation Committee Critical Care Med Examination Board, RCPSC SAQ subcommittee, General Peds Exam Board, RCPSC General Pediatrics Examination Board, RCPSC General Pediatrics Examination Board, RCPSC Editorial Board, International Liaison Committee on Resuscitation (ILCOR) Pediatrics Writing Group, International Liaison Committee on Resuscitation (ILCOR) Pediatrics Task Force, International Liaison Committee on Resuscitation (ILCOR) Policy and Advisory Committee on Resuscitation Heart and Stroke Foundation of Canada 2003 to present Policy and Advisory Committee on Resuscitation Heart and Stroke Foundation of Canada Member 2003 to present International Liaison Committee on Resuscitation (ILCOR) HSFC Representative 2003 to Pediatric subcommittee, American Heart Association HSFC representative 2010- present 2009- present 2009-present 2007- present 2006- present 2002- present 2002- present 2007-present 2007-present 2007- present Chair Member External Surveyor Member Member, marker Member OSCE examiner Member Co-chair, Co-Chair Member present Emergency Cardiac Care Committee EDUCATION AND TRAINING Date Location Training/ Role 1991-1992 Hospital for Sick Children, Toronto, Ontario Pediatric critical care fellow 1990-1991 Chief Resident Pediatrics 1984-1987 Izaak Walton Killam Hospital for Children, Halifax, Nova Scotia Izaak Walton Killam Hospital for Children, Halifax, Nova Scotia University of Calgary 1980-1984 University of Calgary Undergraduate sciences training 1987-1990 Pediatric Resident Medical School EXAMINATIONS, LICENSES, DEGREES 1991 1987 1987 1984 FRCPC (Pediatrics) LMCC MD (University of Calgary) B.Sc. (Biochemistry) University of Calgary COURSES COMPLETED 1994 1992 1991 1991 Pediatric Bronchoscopy course, University N. Carolina A.T.L.S. P.A.L.S. Instructor Course P.A.L.S. PAST MEDICAL EMPLOYMENT (pre-University of Alberta) Date Location Appointment 1992-1993 1992-1993 Department of Pediatrics and Child Health Faculty of Medicine, University of Manitoba Health Sciences Center Winnipeg, Manitoba Winnipeg Children’s Hospital 1992-1993 Manitoba Ambulance Service Medical Advisory 1992-1993 Assistant Professor Primary active staff Pediatric Intensivist/ Emergency Pediatrician Member 1987-1991 Committee Pediatric Residency Training Committee, Department of Pediatrics , Dalhousie University Member MEMBERSHIP IN PROFESSIONAL SOCIETIES Canadian Medical Association Alberta Medical Association Society of Critical Care Medicine Royal College of Physicians and Surgeons of Canada TEACHING: See Teaching Dossier, as well as… University of Alberta 1994-2001 General Pediatrics 2nd yr medical students 1996-97 3rd yr medical students 1995-99 Clinical Teaching Unit preceptor 1998, University of Manitoba 2001 1992-1993 Pediatric Critical Care and Pediatric Emergency Medicine Peds/ Anesthesia/ ER residents American Heart Association Pediatric Advanced Life Support Course Instructor 1990- present Medical Course Director 1995- present Currently medical direct ~3 courses/ year Pediatric Basic Trauma Life Support Course Instructor Medical Course Director 1995- 1997 1995- 1997 Chief pediatrics residency (undergraduate and postgraduate pediatrics teaching) Teaching/ Academic Awards Name of Award Year Body conferring the award Outstanding Teacher-Off Service Rotation Resident Well-Being Award Off Service Rotation of the Year Off Service Rotation of the Year Off Service Rotation of the Year 2008-09 FRCP Emerg Med residency program, U of A 2004-05 2004-05 2002-03 1997-98 Professional Association of Residents of Alberta CFPC- Emerg Med residency program, U of A CFPC- Emerg Med residency program, U of A CFPC- Emerg Med residency program, U of A Off Service Rotation of the Year Pediatrics Rotation of the Year Off Service Rotation of the Year Off Service Rotation of the Year Runner-up, Teacher of the Year Award 1996-9 1996-97 1996-9 1995-96 1992-93 FRCP- Emerg Med residency program, U of A Pediatrics residency program, U of A CFPC- Emerg Med residency program, U of A CFPC- Emerg Med residency program, U of A Pediatrics residency program, U of Manitoba PUBLICATIONS IN PEER REVIEWED JOURNALS/ Book Chapters Shuster, M., J.E. Billi, L. Bossaert, A.R. de Caen, et al. 4: Conflict of interest management before, during, and after the 2010 International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 2010. 81 Suppl 1: p. e41-7. Nolan, J.P., M.F. Hazinski, J.E. Billi, B.W. Boettiger, L. Bossaert, A.R. de Caen, et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation, 2010. 81 Suppl 1: p. e1-25. Morley, P.T., D.L. Atkins, J.E. Billi, L. Bossaert, C.W. Callaway, A.R. de Caen, et al. Part 3: Evidence evaluation process: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 2010. 81 Suppl 1: p. e32-40. Morley, P.T., D.L. Atkins, J.E. Billi, L. Bossaert, C.W. Callaway, A.R. de Caen, et al., Part 3: evidence evaluation process: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation, 2010. 122(16 Suppl 2): p. S283-90. Kleinman, M.E., A.R. de Caen, et al. Advanced Life Support Chapter, Pediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics, 2010. 126(5): p. e1261-318. Kleinman, M.E., A.R. de Caen, et al. Advanced Life Support Chapter, Part 10: pediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation, 2010. 122(16 Suppl 2): p. S466-515. Kleinman, M.E., A.R. de Caen, et al. Part 10: Pediatric Basic and Advanced Life Support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation, 2010. 122(16_suppl_2): p. S466-515. Kleinman, M.E., L. Chameides, S.M. Schexnayder, R.A. Samson, M.F. Hazinski, D.L. Atkins, M.D. Berg, A.R. de Caen, et al. Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics, 2010. 126(5): p. e1361-99. Kleinman, M.E., L. Chameides, S.M. Schexnayder, R.A. Samson, M.F. Hazinski, D.L. Atkins, M.D. Berg, A.R. de Caen. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 2010. 122(18 Suppl 3): p. S876-908. Kleinman, M.E., L. Chameides, S.M. Schexnayder, R.A. Samson, M.F. Hazinski, D.L. Atkins, M.D. Berg, A.R. de Caen, et al. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 2010. 122(18 Suppl 3): p. S876-908. Hazinski, M.F., J.P. Nolan, J.E. Billi, B.W. Bottiger, L. Bossaert, A.R. de Caen, et al. Part 1: executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation, 2010. 122(16 Suppl 2): p. S250-75. de Caen, A.R., M.E. Kleinman, L. Chameides, D.L. Atkins, R.A. Berg, M.D. Berg, F. Bhanji, D. Biarent, R. Bingham, A.H. Coovadia, M.F. Hazinski, R.W. Hickey, V.M. Nadkarni, A.G. Reis, A. Rodriguez-Nunez, J. Tibballs, A.L. Zaritsky, D. Zideman, J. Nolan, B. On behalf of the Paediatric, and C. Advanced Life Support Chapter, Part 10: Paediatric basic and advanced life support 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 2010. Billi, J.E., M. Shuster, L. Bossaert, A.R. de Caen, et al. Part 4: conflict of interest management before, during, and after the 2010 International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation, 2010. 122(16 Suppl 2): p. S291-7. Joffe, A.R., R. Byrne, N.R. Anton, and A.R. Decaen, Donation after cardiac death: a survey of university student opinions on death and donation. Intensive Care Med, 2009. 35(2): p. 240-7. Joffe, A.R., N.R. Anton, and A.R. deCaen, The approach to delayed resuscitation in paediatric cardiac arrest: A survey of paediatric intensivists in Canada. Resuscitation, 2009. 80(3): p. 318-323. Joffe, A.R., R. Byrne, N.R. Anton, and A.R. Decaen, Donation after cardiac death: a survey of university student opinions on death and donation. Intensive Care Med. 2009. 35(2): p. 240-7. Joffe, A.R., N.R. Anton, and A.R. deCaen, Survey of Pediatricians' Opinions on Donation After Cardiac Death: Are the Donors Dead? Pediatrics, 2008. 122(5): p. e967-974. Brierley, J., K. Choong, T. Cornell, A. Decaen, et al. 2007 American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock*. Crit Care Med, 2009; 37(2):666-88. de Caen AR, Reis A, Bhutta A. Vascular Access and Drug Therapy in Pediatric Resuscitation. Pediatr Clin N Am 2008 55 (909-27). de Caen A. Douglas Chamberlain--a man for all decades of his time [Resuscitation 72 (3) 344-349]. Resuscitation. 2008 Mar;76(3):488. Zorzela L, Garros D, de Caen AR. The new guidelines for cardiopulmonary resuscitation: a critical analysis. J Pediatr (Rio J) 2007;83(2 Suppl):S64-S70. de Caen A. Venous access in the critically ill child: when the peripheral intravenous fails! Pediatr Emerg Care 2007;23(6):422-4. de Caen, A., Duff, J., Coovadia, A., Luten, R., Thompson, A., Hazinski, M. Airway Management. In D.G. Nichols (Ed) Rogers’ Testbook of Pediatric Intensive Care. (pp 303-322), Philadelphia, PA: Lippincott Williams & Wilkins, 2007. Hickey R, de Caen A. Warming Procedures, in Textbook of Pediatric Emergency Procedures, 2nd Edition; King C and Henretig FM (ed), pp. 1204-14. Lippincott Williams and Wilkins, 2007. Atkins, D.L., M.D. Berg, R.A. Berg, A.T. Bhutta, D. Biarent, R. Bingham, D. Braner, R. Carrera, L. Chameides, A. Coovadia, A. De Caen, et al. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: Pediatric advanced life support. Pediatrics, 2006. 117(5): p. e1005-e1028. Atkins, D.L., M.D. Berg, R.A. Berg, A.T. Bhutta, D. Biarent, R. Bingham, D. Braner, R. Carrera, L. Chameides, A. Coovadia, A. De Caen, et al. The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: Pediatric basic and advanced life support. Pediatrics, 2006. 117(5): p. e955-e977. Atkins, D.L., M.D. Berg, R.A. Berg, A.T. Bhutta, D. Biarent, R. Bingham, D. Braner, R. Carrera, L. Chameides, A. Coovadia, A. De Caen, et al. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: Pediatric basic life support. Pediatrics, 2006. 117(5): p. e989-e1004. Singhal N, De Caen A. The authors respond [2]. Paediatrics & Child Health 2006;11(5):270. Shuster M, de Caen A, Gay M. Emergency cardiovascular care guidelines 2005. Can Fam Physician 2006;52:480-2. de Caen, A. Singhal, N. A Summary of the Changes in Pediatric Resuscitation Guidelines stemming from the International CoSTR Document, Paediatrics and Child Health. 2006. 11(1): p. 11-13. de Caen, A., Management of profound hypothermia in children without the use of extracorporeal life support therapy. Lancet, 2002. 360(9343): p. 1394-5. ABSTRACTS/ POSTER PRESENTATIONS Joffe AR., Byrne R, Anton NR, deCaen AR. A survey of university student opinions about donation after cardiac death. American Thoracic Society, Toronto, Ontario; May 2008. Published in: Am J Resp Crit Care Med 2008;111:A515. Joffe AR, Byrne R, Anton NR, deCaen AR. A survey to determine philosophy student opinions about donation after cardiac death: it matters how you ask the question. Critical Care Canada Forum; Toronto, Ontario, October 29-Nov1 2007. Resp Crit Care Med 2008;111:A515. Joffe AR, Byrne R, Anton NR, deCaen AR (2007) A survey to determine medical student opinions about donation after cardiac death. Pediatr Crit Care Med 8:A186. 27. Joffe AR, Byrne R, Anton NR, deCaen AR (2007) A survey to determine nursing student opinions about donation after cardiac death: it matter how you ask the question. Pediatr Crit Care Med 8:A187. Joffe AR, Byrne R, Anton NR, deCaen AR. A survey to determine medical student opinions about donation after cardiac death: it matters how you ask the question. 5th World Congress on Pediatric Critical Care; Geneva, Switzerland; July 2007. Joffe AR, Byrne R, Anton NR, deCaen AR. A survey to determine nursing student opinions about donation after cardiac death: it matters how you ask the question. 5th World Congress on Pediatric Critical Care; Geneva, Switzerland; July 2007. de Caen, Allan, Intraosseous access is safe, effective for fluid resuscitation, drug delivery and laboratory evaluation and attainable in all age groups 2005 International Consensus on CPR and ECC Science with Treatment Recommendations Dallas, January 2005 http://www.americanheart.org/presenter.jhtml?identifier=3026177 de Caen, Allan, Dosing with select endotracheal medications (epinephrine, atropine, lidocaine, naloxone or vasopressin) is an efficient and clinically effective option in the setting of failed intravenous access in the child with cardiac arrest, shock or respiratory failure 2005 International Consensus on CPR and ECC Science with Treatment Recommendations Dallas, January 2005 http://www.americanheart.org/presenter.jhtml?identifier=3026177 de Caen, Allan, Vasoactive agents improve hemodynamics and outcome in the setting of post-arrest myocardial dysfunction. 2005 International Consensus on CPR and ECC Science with Treatment Recommendations Dallas, January 2005 http://www.americanheart.org/presenter.jhtml?identifier=3026177 A de Caen, I Rebeyka, A Joffe. Management of Profound Hypothermia in Children <20C (Core Body T) Without Using ECLS Therapy. accepted for poster presentation at 2001 Pediatric Critical Care Colloquium, San Diego B Van Skiver, A. de Caen, I Chaykowski., Cellular phone transmissions interference with transport medical equipment function. Poster presentation at the World Congress of Pediatric Intensive Care, Montreal June, 2000. Reviewer for Journals Resuscitation Pediatrics Journal of Clinical Anesthesia Canadian Medical Association Journal Grant Reviewer SickKids Foundation (HSC Toronto) INVITED SPEAKER (external to University of Alberta) Date/ Location Duration Title Description June 5, 2011 Edmonton, Canada April 7-9, 2011 Alexandria, Egypt 1 hr Management of Environmental Hypothermia: Is ECLS an option? SEECMO ECMO Conference multiple Invited Speaker at 3rd International PICU Conference March 13-17, 2011 Sydney, Australia multiple Jan 23, 2011 Banff, Canada 11/2 hrs 1) AHA PALS 2010 Resuscitation Guidelines changes 2) Pediatric Cardiac Arrest: Physiology, Epidemiology and Management 3) Pediatric ARDS 1) Expert Panels on Resuscitation: Expert Panel 2) New Resuscitation Guidelines and Key Changes: Where are we now? ECC CPR Guideline Changes for Pediatric and Adult Populations Dec 8, 2010 Miami, USA 20 min PALS 2010: What’s New? Oct 23, 2010 Calgary, Canada Sept 6-19, 2009 Beijing, China 1 hr New PALS Guidelines Pediatric Cardiac Intensive Care Society 8th International Conference Alberta Medical Association Pediatrics Section Sept-Dec 2010 1 hr X 4 Invited Speaker at 6th World Congress on Pediatric Critical Care U of Calgary’s 27th Annual Emergency Medicine for Rural Hospitals: A program for physicians and nurses Invited faculty (PICU) on International Children’s Heart Foundation mission to Beijing Children’s Hospital New Pediatric Resuscitation 4 lectures for AHS Guidelines for Alberta’s Paramedics paramedics, Edmonton, AB March 18, 2009 30 min Osaka, Japan Nov 9-21, 2009 Kiev and Kharkov, Ukraine Oct 21, 2008 1 hr Edmonton, Canada Pediatric Medical Emergency Teams Oct 8-22, 2007 Hangzhou, China Invited faculty (PICU) on Stollery Cardiac Surgical mission to Hangzhou, China The 2006 Pediatric Resuscitation Canadian Society of Guidelines for the RT Respiratory Therapists National Forum 2007 June 1, 2007 Montreal, Canada 1 hr June 1, 2007 1 hr Japanese Resuscitation Council Scientific Meeting Invited faculty (PICU) on International Children’s Heart Foundation mission to 2 Cardiac ICU centres in Ukraine Transport Systems Moving our CAPHC 2009 Annual Meeting Children Across Systems – Challenges, Barriers and Enablers Pediatric ARDS: An Evidence Based Canadian Society of Montreal, Canada April 25, 2007 Edmonton, Canada Approach 1 hr Respiratory Therapists National Forum 2007 Resuscitation Guidelines and Changes 2007 Pediatric Critical Care: to PALS Practice Setting the Standards Pre-Conference Symposium Conference March 10, 2007 30 min Johannesburg, South Africa Venous Access in the Critically Ill Child International Resuscitation - When Peripheral IV Fails and Emergency Cardiovascular Care Symposium March 10, 2007 30 min Johannesburg, South Africa Emergency Care of the Paediatric Burn International Resuscitation Patient and Emergency Cardiovascular Care Symposium Jan 26, 2007 Edmonton, Canada 1 hr Hypovolemic Shock Nov 7, 2006 Edmonton, Canada 1 hr Oct 15-29, 2006 Minsk, Belarus Shock Talk: A workshop for Pediatric Health Care Professionals Stollery Children’s Hospital The Science Behind the New PALS Edmonton EMS Rounds – Guidelines Symposium Invited faculty (PICU) on International Children’s Heart Foundation mission to 2 Cardiac ICU centres in Minsk, Belarus 2006 Revised American Heart American Academy of Association Guidelines on Emergency Pediatrics National Cardiovascular Care and CPR Conference and Exhibition “Airway” Oct 7, 2006 Atlanta, USA 15 min May 26, 2006 Toronto, Ontario 1 hr Pediatric Resuscitation: 2005 HSFC & 2006 HSFC National AHA PALS Guidelines Resuscitation Conference March 4, 2006 Mississauga, Ontario 1 hr Pediatric Critical Care Pearls Pediatric Review Course 2006 January 21, 2006 Banff, Canada 1 hr Management of the Child in Shock University of Calgary’s 22nd Annual Emergency Medicine for Rural Hospitals January 21, 2006 Banff, Canada 1 hr Adult and Pediatric Resuscitation University of Calgary’s 22nd Guidelines Annual Emergency Medicine for Rural Hospitals November, 2005 Edmonton, Canada 1 hr Pediatric Transport and the RT June 2005 1 hr Pediatric & Neonatal Resuscitation: The CARTA (Alberta Respiratory Therapy) Meeting International Montreal, Canada The Science leading up to the 2005 Interdisciplinary Conference CoSTR Document on Emergencies June 2005 Montreal, Canada 1 hr Pediatric & Neonatal Resuscitation: The International The Science leading up to the 2005 Interdisciplinary Conference CoSTR Document on Emergencies April 2005 Edmonton, Canada 1 hr Pediatric Trauma: Transport Style Pediatric Critical Care: Issues in Trauma and Cardiovascular Care January 23-29, 2005 Dallas, USA 20 min Intraosseous access is safe, effective for fluid resuscitation, drug delivery and laboratory evaluation and attainable in all age groups. January 23-29, 2005 Dallas, USA 20 min January 23-29, 2005 Dallas, USA 20 min Dosing with select endotracheal medications (epinephrine, atropine, lidocaine, naloxone or vasopressin) is an efficient and clinically effective option in the setting of failed intravenous access in the child with cardiac arrest, shock or respiratory failure Vasoactive agents improve hemodynamics and outcome in the setting of post-arrest myocardial dysfunction. International Consensus on ECC and CPR Science with Treatment Recommendations, Taskforce: Pediatric Life Support: International Liaison Committee on Resuscitation International Consensus on ECC and CPR Science with Treatment Recommendations, Taskforce: Pediatric Life Support: International Liaison Committee on Resuscitation November, 2005 Edmonton, Canada 1 hr `Pediatric Transport and the RT Oct 2004 Porto Alegre, Brazil 3 hrs PALS: Does it Make a Difference in 6th Latin-American Congress Outcome? of Pediatric Intensive Care PALS 2005: What is new ? Vasopressin and Pediatric Shock/ Cardiac Arrest November, 2003 Edmonton, Canada 1 hr Pediatric Hypothermia Pediatric Emergency Medicine Conference June, 2002 Edmonton, Canada 1 hr Pediatric Hypothermia ER/ Critical Care Conference: Innovative Medical Concepts 1999 Jasper, Canada 1 hr Pediatric Resuscitation 4th Annual Rural Emergency Medicine Update International Consensus on ECC and CPR Science with Treatment Recommendations, Taskforce: Pediatric Life Support: International Liaison Committee on Resuscitation CARTA (Alberta Respiratory Therapy) Meeting 1999 Edmonton, Canada 1 hr Little Medical Problems Interphase National Conference 1999 Edmonton, Canada 1998 Edmonton, Canada 1996 Edmonton, Canada 1996 Peace River, Canada 1 hr Pediatric Transport 1 hr Approach to the Critically Ill Infant Interphase National E.M.S. Conference C.T. Fried Pediatrics Conference 1 hr Resuscitation and Stabilization of the S.T.A.R.S. Outreach Medical Sick Child Education video Approach to the Critically Ill Infant Peace River Emergency Medicine and EMS Conference 1995 Edmonton, Canada 1994 Banff, Canada 1 hr Respiratory Distress in the Infant 1 hr Pediatric Analgesia 1 hr E.M.S. C.T. Fried Pediatrics Conference Banff Seminar, Western Branches, Canadian Society of Hospital Pharmacists Speaker (within Dept of Pediatrics, University of Alberta) Date/ Location Nov 4, 2010 Duration 1 hr Title Pediatric Resuscitation Science: The New HSFC/ AHA PALS Guidelines PALS update (2006 Resuscitation Guidelines) Description Dept of Pediatrics Grand Rounds UAH Emergency Dept. Nursing Education Update Day PALS Guidelines Update 2006 Dept of Pediatrics Grand Rounds PALS update (2006 Resuscitation Ped Emergency Medicine Guidelines) Grand Rounds May 25, 2006 1 hr Jan 12, 2006 1 hr Jan 12, 2006 1 hr Feb 7, 2006 1 hr April 25, 2002 1 hr November 28, 2001 1 hr Management of the Critically Ill Grey Nuns Hospital Pediatrics Asthmatic Grand Rounds: April 27, 2000 1 hr Meningococcal Disease: Dept of A Pediatric Intensivist’s Perspective Rounds PALS/ ACLS Update at ER Rounds Division of Emergency MedicineGrand Rounds Pediatric Critical Care Transport: Dept of Pediatrics Grand A Northern Alberta Perspective Rounds Pediatrics Grand Invited Clinical Faculty Pediatric Intensivist International Children’s Heart Foundation Cardiac Surgical Mission Beijing, China Sept 5-19, 2008 Pediatric Intensivist International Children’s Heart Foundation Cardiac Surgical Mission Kiev and Kharkov, Ukraine Nov 9-22, 2008 Pediatric Intensivist Stollery Childrens’ Hospital Pediatric Cardiac Surtgical Mission Hangzhou, China Oct 8-22, 2007 Pediatric Intensivist International Children’s Heart Foundation Cardiac Surgical Mission Minsk, Belarus Oct 14-28, 2006 Pediatric Resident Mentor Dept of Pediatrics Mentorship Program 2005-present
Scaricare