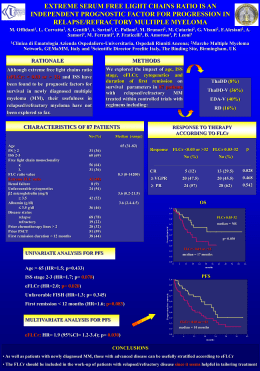
Le metastasi cerebrali Nuove classi di rischio e sopravvivenza Antonio Silvani UOC Neurologia 2- Neuro-oncologia Dipartimento di Neuro-oncologia 23 aprile 2015 Hotel Palace Como Number of metastases Factors Used to Assess Therapy Patient’s input Age / KPS Therapy Primary tumor / stage Extracranial disease Neurological deficits Size of lesion(s) • Location Patients with brain metastases comprise a heterogeneous patient population In many patients with brain metastases, the primary therapeutic aim is symptom palliation and maintenance of neurologic function, but in a subgroup, long-term survival is possible More accurate prognostic information may support the decision making process and treatment recommendations for these patients RPA: Recursive Partitioning Analysis SIR: Score Index Radiosurgery Five major indices BSBM: Basic score for brain metastases GPA: Graded Prognostic Assessment Modified RPA Able to carry on normal activity and to work; no special care needed. Unable to work; able to live at home and care for most personal needs; varying amount of assistance needed. Unable to care for self; requires equivalent of institutional or hospital care; disease may be progressing rapidly. 100 Normal no complaints; no evidence of disease. 90 Able to carry on normal activity; minor signs or symptoms of disease. 80 Normal activity with effort; some signs or symptoms of disease. 70 Cares for self; unable to carry on normal activity or to do active work. 60 Requires occasional assistance, but is able to care for most of his personal needs. 50 Requires considerable assistance and frequent medical care. 40 Disabled; requires special care and assistance. 30 Severely disabled; hospital admission is indicated although death not imminent. 20 Very sick; hospital admission necessary; active supportive treatment necessary. 10 Moribund; fatal processes progressing rapidly. 0 Dead KARNOFSKY PERFORMANCE STATUS SCALE : KPS RTOG 85-28 RPA tree 1200 BM pts RTOG 79-16 RTOG 89-05 Brain Metastases: Recursive Partitioning Analysis Gaspar L et al. Int J RadiatOncol Biol Phys. 1997 Class I Class II KPS ≥ 70 KPS ≥ 70 Primary controlled Primary uncontrolled Class III KPS <70 Age < 65 Age ≥ 65 No extracranial MTS extracranial MTS Performance status and active extracranial disease as major indicators of outcome following therapy Brain Metastases: Recursive Partitioning Analysis Gaspar L et al. Int J RadiatOncol Biol Phys. 1997 Class I Class II KPS ≥ 70 KPS ≥ 70 Primary controlled Primary uncontrolled Class III KPS <70 Age < 65 Age ≥ 65 No extracranial MTS extracranial MTS MST 7.1 mons MST 4 .2 MST 2.3 mons 20% 65% 15 % Recursive Partitioning Analysis (RPA) Classification Predicts Survival in Patients with Brain Metastases from Sarcoma Grossman G World Neurosurg. 2014 Radiographically distinct on MRI/CT Favorable Characteristics of Brain Metastases for SRS Pseudospherical shape Displaces normal brain tissue Minimal invasion of normal brain Size at presentation ≤3 cm SIR Index RPA SIR Index 0 1 2 Age Age yrs ≥ 60 51-59 ≤ 50 KPS KPS ≤ 50 60-70 >70 Systemic disease st Systemic disease status PD PR–SD CR–NED Largest lesion volume cm3 >13 5-13 <5 Number of lesions ≥3 2 1 Extracranial mts Basic score for brain metastases (BS-BM) Score Variable 0 1 50-70 80-100 Control of primary tumor No Yes Extracranial MTS Yes No KPS Graded Prognostic Assessment (GPA) for brain metastases Sperduto P Int J Radiat Oncol Biol Phys 70:510, 2008 To incorporate new data from RTOG9508 that showed the number of metastases to be prognostic To eliminate treatment factors because the point of a prognostic index is to guide treatment choice, rather than reflect treatment results Rationale To eliminate components that are difficult to quantify and/or subjective, such as control of extracranial disease GPA Graded Prognostic Assessment (GPA) for brain metastases Sperduto P Int J Radiat Oncol Biol Phys 70:510, 2008 RPA SCORE-GPA Age KPS Extracranial mts 0 0.5 1 Age >60 50-69 <50 KPS <70 70-80 90-100 Number of CNS metastases >3 2-3 1 Extracranial mts Present Systemic Status disease SCORE Median Survival 3.5-4 11.0 mons 3 6.9 1.5-2.5 3.8 0-1 2.6 None Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None GPA: 2.5 OS: 3.8 mts ‘Subtype’ Luminal A’ ER and/or PgR positive HER2 negative Ki-67 low (<14%) Breast cancer: Systemic treatment recommendations for subtypes ‘Luminal B (HER2 positive)’ ‘ER and/or PgR positive Any Ki-67, HER2 overexpressed or amplified HER2 positive (non luminal) HER2 over-expressed or amplified ER and PgR absent Triple negative (basal)’ Type of therapy Notes on therapy Endocrine therapy alone Few require cytotoxics (e.g. high nodal status or other indicator of risk: No data are available to Cytotoxics + anti-HER2 + support the omission of endocrine therapy cytotoxics in this group Cytotoxics + anti-HER2 Cytotoxics Patients at very low risk (e.g. pT1a and node negative) may be observed without systemic adjuvant treatment. Lung Are prognostic factors the same in different histologies ? Age x KPS x ECM x NoBM x Subtype Melanoma Breast Renal GI x x x x x x x x x Graded Prognostic Assessment (GPA) worksheet to estimate survival from brain metastases (BM) by diagnosis Paul W. Sperduto et al. JCO 2012;30:419-425 Breast Kaplan-Meier curves for survival for six diagnoses by Graded Prognostic Assessment (GPA) group, SCLC Renal ca Paul W. Sperduto et al. JCO 2012;30:419-425 NSCLC Melanoma GI ca Prognostic factors 0 0.5 1.0 1.5 2.0 ≤50 <60 70-80 90-100 na Subtype basal na LumA Her2 LumbB Age ≥60 ≤60 na na na KPS GPA worksheet to estimate survival from brain metastases in breast cancer Paul W. Sperduto JNO 2013 Total Subtype Basal Triple Negative (ER/PR/HER2-neg) LuminalA ER/PR-pos, HER2-neg Luminal B Triple Positive, ER/PR/HER2-pos Her-2 HER2-pos, ER/PR-neg Score 60 50 The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer PW Sperduto JNO2013 40 30 20 10 0 Basal Her2 Median months from primary DX to brain METS Luminal B Luminal A MST in months from brain MET treatment http://brainmetgpa.com NSCLC Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None NSCLC Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None NSCLC Age 67 KPS 90-100 Number of CNS metastases: 3 Extracranial metasteses None NSCLC Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None NSCLC Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None NSCLC Age 67 KPS 70-80 Number of CNS metastases: 3 Extracranial metasteses None http://brainme tgpa.com Exeresis 14 dec 2014 SRT CHT April 2 Adenocarcinoma Large Cell Squamous P value GPA 3.5–4.0 11.2 4.1 10.6 0.8597 GPA 3 12.1 10.2 6.9 0.0420 GPA 1.5-2.5 6.1 4.6 3.6 0.0052 GPA 0-1 3.2 2.2 3.2 0.0205 412 newly diagnosed patients treated outside of clinical trials 1983-2011 “typical patient populations that many oncologists in Europe will face in everyday practice are different from those included in the multi-institutional database (11 institutions from the United States and Canada, time period 1985 to 2007” More than 50% of patients in each diagnosis stratum had surgery or radiosurgery (SRS) as a component of treatment, except for those with small-cell lung cancer (whole-brain radiotherapy Nieder Sperduto 2012 412 (yrs 1983-2011) 3940 (yrs 1985-2007) NSCLC+Melanoma 69% 67% Surgery or SRS ± WBRT 19% 45% Worst Group 0-1 points 36 % 16 % Best Group 3-5 points 7% 14% Median survival months 3.6 7.2 7 13.8 2.7 3.1 Pts Median survival breast Median survival 0–1 points Primary tumour type Nieder Sperduto Lung cancer KPS, age KPS, age, number of BM, extracranial metastases Breast cancer KPS KPS, age, histology Renal cell cancer Extracranial metastases, number of BM KPS, number of BM Gastrointestinal primary KPS, extracranial metastases, KPS number of BM Malignant melanoma KPS, number of BM KPS, number of BM The real-world utility of predictions Questions 1 How do the many clinical pieces of information result in a prediction, and how accurate is that prediction? 2 Does the survival expectation differ among medical specialties? 3 How often is our expectation very wrong? 4 Are clinicians overly optimistic, fairly accurate, or nihilistic? NSCLC breast Grazie per l’attenzione Antonio Silvani [email protected]
Scaricare