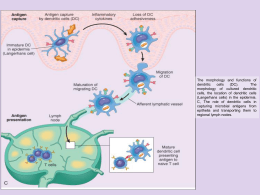
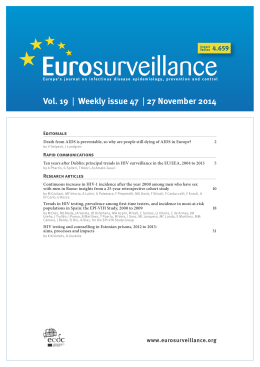
Tubercolosi, HIV e migrazione: una reale emergenza? SESSIONE II -ˇ HIV e Tubercolosi nella persona immigrata Miriam Lichtner Dipartimento di Malattie Infettive e Sanità Pubblica Sapienza Università di Roma Polo Pontino Componente dell’ Italian National Focal Point – Infectious Diseases and Migrant” Sergej • Dopo 4 mesi di ART e 2 di anti-TB (11/04/07): febbre elevata con sospetto di IRIS, inizia deltacortene e streptomicina • CD4+ 98/mmc, HIV-RNA<50 • Dimissione 26/4/07 controllo DH dopo 1 sett IRIS: Quadri storici di IRIS • Reazione paradossale nella TB dopo inizio trattamento • Reazione infiammatoria nei pz con lebbra in trattamento • Recupero del sist. immune dopo trapianto di midollo e chemioterapia • Risposta atipica infiammatoria ai micobatteri atipici nei pz in terapia con AZT (anni 80) 6 Antiretroviral Therapy Improves Qualitative and Quantitative Immune Defects Immune suppression/deficiency HIV replication Immune activation Qualitative/functio nal immune defects Quantitative immune defects Response to recall antigens CD4 counts Impaired pathogen -specific immunity OI Immune Reconstitution HAART HIV replication Immune activation Migueles, Buenos Aires 2003 Qualitative/function al immune defects Quantitative immune defects Reversal of anergy Redistribution, death (HIV-, activation-induced), production (peripheral expansion and thymic) Lymphocyte proliferative capacity Improved pathogenspecific immunity Improved immune control 7 Immune reconstitution inflammatory syndrome Patients Started on ART 2330 Immune reconstitution syndrome 302 85 HERPES ZOSTER 81 TUBERCULOSIS 72 CMV RETINITIS 31 PCP 28 CRYPTOCOCCOSIS HANSEN'S 3 OTHERS 3 Source: GHTM, Chennai 8 Defining IRIS Required criterion Supportive criterion Worsening symptoms of inflammation/infection Increase in cd4 cell count of > 25 cells/cu.mm Temporal relationship with starting Biopsy demonstrating well formed antiretroviral treatment granulomatous inflammation or unusually exuberant inflammatory response Symptoms not explained by newly acquired infection or disease or the usual course of a previously acquired disease > 1 log10 decrease in plasma viral load Source: CID J 2006;(1 June) 42: 1639-46 9 Defining IRIS • Proposed criteria for the diagnosis of IRIS • HIV positive • Receiving HAART – Decrease in HIV-1 RNA level from baseline – Increase in CD4 cells from baseline(may lag HIV-1 RNA decrease) • Clinical symptoms consistent with inflammatory process • Clinical course NOT consistent with: – Expected course of previously diagnosed OI – Expected course of newly diagnosed OI – Drug toxicity Source:10Journal of Antimicrobial Chemotherapy (2006) 57, 167-170; Samuel A. Shelburne, Martin Montes and Richard J.Hamill Defining IRIS: Major Criteria • Previous diagnosis of AIDS • Concurrent Antiretroviral Therapy; Increase in CD4 count and Decrease in plasma vireamia by > 1 log copies/ml • Atypical presentation of ‘opportunistic infection or tumor’ i.e. – – – – – localized disease or exaggerated inflammation or atypical inflammatory response or worsening of pre existing disease. Symptoms consistent with infectious/inflammatory condition • Symptoms not explained by normal course of previous or new OI or side effect of ART 11 Source: Battegay and Drechsler; Current Opinion in HIV and AIDS; 2006, 1; 56-61 Defining IRIS: Minor Criteria • Increase in CD4 cell count • Increase in measured specific immune response • Spontaneous resolution of symptoms without specific therapy Source: Battegay and12 Drechsler; Current Opinion in HIV and AIDS; 2006, 1; 56-61 Onset of IRIS 13 Source: AIDS 2005, Vol 19 No4 ;399-406, Samuel A. Shelburne et al Risk factors • Risk factors at base line: – Lower CD4 count prior to start of ART – Higher HIV-1 RNA levels at base line – Initiating ART in close proximity to starting therapy for an OI • Response to therapy & the development of IRIS: – Rapid fall in HIV-1 RNA level during the first 3 months of therapy Source: Journal of Antimicrobial Chemotherapy (2006) 57, 167-170;Samuel A. Shelburne, Martin Montes and Richard J.Hamill 14 Risk factors for IRIS Microbial antigens Host susceptibility CD4< 50 Adapted from French et al, 2004 15 Management • Mild form (with ongoing ART) – Observation • Localized IRIS (with ongoing ART) – Local therapy such as minor surgical procedures for lymph node abscesses • Most of the situations (with ongoing ART) – Unmasking &/or Recognition of ongoing infections >> Antimicrobial therapy to reduce the antigen load of the triggering pathogen; – Reconstituting immune reaction to non-replicating antigens >> no antimicrobial therapy. Short term therapy with corticosteroids or non-steroidal anti inflammatory drugs to reduce the inflammation. 16 Management • Temporary cessation of ART has to be considered if potentially life threatening forms of IRIS develop 17
Scaricare