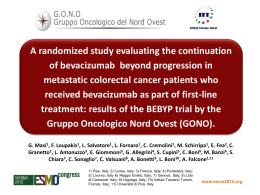
American Society of Clinical Oncology Annual Meeting 2010 Chicago, Illinois - June 04-08, 2010 FOLFOXIRI plus bevacizumab (BV) vs FOLFIRI plus BV as firstline treatment of metastatic colorectal cancer (MCRC): preliminary safety results of the phase III randomized “TRIBE” study by the Gruppo Oncologico Nord-Ovest (GONO). Alfredo Falcone 1,2, Fotios Loupakis 1,2, Samanta Cupini3, Enrico Cortesi4, Angela Buonadonna5, Gianluca Tomasello6, Maria Banzi7, Monica Ronzoni8, Alberto Zaniboni9, Gianluca Masi1,2. 1. U.O. Oncologia Medica 2 Universitaria, Azienda Ospedaliero-Universitaria Pisana, Istituto Toscano Tumori, Pisa, Italy; 2. Dipartimento di Oncologia, dei Trapianti e delle Nuove Tecnologie in Medicina, Università di Pisa, Italy; 3.U.O.Oncologia Medica, Azienda USL-6, Istituto Toscano Tumori, Livorno, Italy ; 4. Dipartimento di Oncologia Medica, Università di Roma La sapienza, Roma, Italy ; 5. Dipartimento di Oncologia Medica, Istituto Nazionale Tumori, Aviano, Italy; 6. Divisione di Medicina e Oncologia Medica, Azienda Istituti Ospitalieri di Cremona, Cremona, Italy; 7. Arcispedale Santa Maria Nuova, Reggio Emilia, Italy; 8. Dipartimento di Oncologia, Istituto Scientifico San Raffaele, Milano, Italy; 9. Fondazione Poliambulanza, Brescia, Italy Rationale The combination of BV with cytotoxic drugs is an efficacious strategy in the treatment of mCRC. Hurwitz H, N Eng J Med 2004 Giantonio B, J Clin oncol 2007 Saltz L, J Clin Oncol 2008 The triple drug combination FOLFOXIRI demonstrated increased activity and efficacy over FOLFIRI in a randomized trial. Falcone A, J Clin Oncol 2007 The combination of FOLFOXIRI plus BV demonstrated promising results in phase II. Masi G, ESMO 2009 Study Design Stratification • Center • PS 0 vs 1-2 • Adjuvant CT R A N D O M FOLFIRI + BV 5-FU + BV FOLFOXIRI + BV 5-FU + BV INDUCTION TX MAINTENANCE TX • up to 12 cycles • until PD • or PD • or intolerable toxicity • or unacceptable • or patient’s refusal toxicity • or patient’s refusal FOLFOXIRI + BEVACIZUMAB: INDUCTION SCHEDULE Day 1 Day 2 & Day 3 BV 5 mg/Kg CPT-11 165 mg/sqm Oxaliplatin 85 mg/sqm L-LV 200 mg/sqm 5FU flat continuous infusion 3200 mg/sqm 30 min 1 hour 2 hours Repeated every 2 weeks 48 hours FOLFIRI + BEVACIZUMAB: INDUCTION SCHEDULE Day 1 Day 2 & Day 3 BV 5 mg/Kg CPT-11 180 mg/sqm L-LV 200 mg/sqm 30 min 90 min 5FU bolus 5FU flat continuous infusion 400 mg/sqm 2400 mg/sqm bolus Repeated every 2 weeks 48 hours 5FU/LV + BEVACIZUMAB: MAINTENANCE SCHEDULE Day 1 Day 2 & Day 3 BV 5 mg/Kg L-LV 200 mg/sqm 5FU flat continuous infusion 2400 - 3200 mg/sqm 30 min 90 min 48 hours Repeated every 2 weeks Maintenance Treatment: Schedules INDUCTION TX MAINTENANCE TX 5-FU/LV + BV FOLFIRI + BV BV 5 mg/kg 30-min d.1 L-LV 200 mg/m2 2-h d.1 5FU 400 mg/m2 bolus d.1 5FU 2400 mg/m2 46-h CI d.1 q. 2 wks x 12 cycles 5-FU/LV + BV FOLFOXIRI + BV BV 5 mg/kg 30-min d.1 L-LV 200 mg/m2 2-h d.1 5FU 3200 mg/m2 48-h CI d.1 q. 2 wks x 12 cycles Study Objectives PRIMARY Progression free survival SECONDARY Overall response rate Duration of response R0 surgery of metastases Overall survival Safety profile Potential markers predictive of bevacizumab activity Main inclusion criteria • Histologically proven metastatic colorectal cancer • Not resectable disease • Not previous chemotherapy for metastatic disease • At least one measurable lesion according to RECIST criteria • Age 18-75 years • ECOG PS ≤ 2 if age < 71 years; ECOG PS = 0 if aged 71-75 years • Previous adjuvant therapy containing oxaliplatin or bevacizumab is allowed if more than 12 months have elapsed between the end of adjuvant therapy and first relapse Main exclusion criteria • History or evidence of CNS disease unless adequately treated • Serious, non-healing wound, ulcer, or bone fracture • Evidence of bleeding diathesis or coagulopathy • Clinically significant cardiovascular disease (cerebrovascular accidents ≤6 months, myocardial infarction ≤ 6 months, unstable angina, NYHA grade II or greater congestive heart failure, serious cardiac arrhythmia requiring medication). • Uncontrolled hypertension • Treatment with anticoagulants for therapeutic purposes • Major surgical procedure, open biopsy, or significant traumatic injury within 28 days prior to study treatment start Statistics The primary study end-point is Progression Free Survival Previous trials have shown that the median PFS of MCRC pts treated in first-line with bevacizumab in combination with a fluoropyrimidine-based doublet (as FOLFIRI) is about 11 months. With the use of a two-sided, unstratified log-rank test with a type I error of 0.05, we determined that 379 events (disease progression or death from any cause) would be required for an 80% power to detect a hazard ratio for progression of 0.75. With a 1:1 randomization of assignment to study groups and considering a total duration of the study of 54 months we estimated that we would need to enroll 450 patients to observe 379 events. The primary statistical analysis of efficacy will be the performed according to the intention-to-treat principle. Dose Reductions and Delays Criteria: Chemotherapy AT THE START OF CYCLE GRADE WBC < 3.000/mm3 Neutrophils < 1.000/mm3 CPT-11 LOHP 5-FU Platelets < 100.000/mm3 Diarrhea ≥1 Mucositis ≥1 Any other NHT ≥2 HFS 3-4 100% 100% STOP Neurotoxicity ≥3 100% STOP 100% GRADE CPT-11 LOHP 5-FU Febrile neutropenia 4 75% 75% 100% Thrombocytopenia 3-4 75% 75% 100% Diarrhea 3 75% 100% 75% Diarrhea 4 50% 100% 50% Mucositis 3 100% 100% 75% Mucositis 4 100% 100% 50% PREVIOUS TOXICITY HOLD UNTIL RESOLUTION Dose Reductions and Delays Criteria: Bevacizumab TOXICITY GRADE BV Hypertension 3 STOP if uncontrolled despite appropriate tx Hypertension 4 STOP Hemorrhage 2-3 HOLD UNTIL RESOLUTION Hemorrhage 4 STOP Venous thrombosis 3-4 STOP Arterial thrombosis Any STOP Congestive heart failure 3 HOLD UNTIL GRADE ≤2 Congestive heart failure 4 STOP Proteinuria 3 HOLD UNTIL GRADE ≤2 Proteinuria 4 STOP GI perforation Any STOP Wound dehiscence Any STOP Safety Interim Analysis At the time of the present analysis, 268 patients have been enrolled into the study: Arm A: FOLFIRI + BV: 133 Arm B: FOLFOXIRI + BV: 135 The objective of this interim analysis is to evaluate safety among the first 150 patients enrolled: Arm A: FOLFIRI + BV: 74 Arm B: FOLFOXIRI + BV: 76 All toxic events are graded according to NCI-CTC version 3.0. Patients Characteristics FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts Age, median (range) 59 (29-74) 58 (29-74) Sex M/F 51% / 49% 59% / 41% ECOG PS 0/1-2 89% / 11% 87% / 13% Primary Colon/Rectum 69% / 31% 72% / 28% 26% 22% Sites of mts 1/≥2 23%/77% 34% /66% Previous adjuvant CT Y/N 11% / 89% 11% / 89% Previous adjuvant RT Y/N N. of induction treatment cycles administered Median N. of induction treatment cycles per patient 7% / 91% 3% / 93% 714 724 12 11 Primary on site Maximum Per Patient Non-Haematological Toxicities during INDUCTION TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts G1-2 G3-4 G1-2 G3-4 Nausea 57% 1% 51% 4% Vomiting 20% 0% 30% 5% Diarrhea 46% 8% 50% 20% Stomatitis 39% 5% 45% 9% Asthenia 46% 8% 59% 7% Hand-Foot Syndrome 11% 0% 12% 0% Neurotoxicity (grade 2-3) NA 22% Maximum Per Patient Haematological Toxicities during INDUCTION TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts G1-2 G3-4 G1-2 G3-4 24% 14% 22% 47% Febrile Neutropenia - 4% - 7% Thrombocytopenia 8% 1% 22% 3% Anemia 51% 0% 62% 1% Neutropenia Maximum Per Patient Cardiovascular Toxicities during INDUCTION TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts G1-2 G3-4 G1-2 G3-4 Hypertension 22% 1% 17% 1% Bleeding 27% 0% 29% 3% Venous thrombosis 0% 8% 3% 9% Arterial thrombosis 0% 1% 0% 3% GI perforation 0% 0% 0% 1% Proteinuria 19% 1% 22% 1% Ematuria 8% 1% 9% 0% Maximum Per Cycle Toxicities during INDUCTION TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts 714 724 N. of cycles administered G1-2 G3-4 G1-2 G3-4 Diarrhea 22% 1% 26% 3% Stomatitis 13% 1% 14% 1% Neutropenia 10% 3% 22% 11% Febrile Neutropenia - 1% - 1% Thrombocytopenia 3% 1% 8% 1% Serious Adverse Events (during INDUCTION Treatment) FOLFIRI 74 pts All SAE Type of Serious Adverse Events 11 pts (15%) FOLFOXIRI 76 pts 15 pts (20%) 1 Stroke 1 Cardiac Ischemia 1 Sudden Death 2 Atrial Flutter 2 Pulmonary Embolism 1 Sepsis 1 Deep Vein Thrombosis 1 Pneumonia 1 GI Bleeding 1 GI Bleeding 1 GI Obstruction 1 GI Perforation 3 Diarrhea 6 Diarrhea 1 Febrile Neutropenia 2 Febrile Neutropenia Possibly Tx-related Deaths (during INDUCTION Treatment) * based on investigators’ judgment FOLFIRI 74 pts Possibly Treatment Related Deaths* 3 pts (4%) FOLFOXIRI 76 pts 2 pts (3%) 1 Stroke 1 GI bleeding 2 Pulmonary Embolism 1 Sepsis Dose Reductions and Treatment Delays due to Toxicities during INDUCTION TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts • 5-Fluorouracil 5% 6% • Irinotecan 5% 9% • Oxaliplatin NA 9% • 5-Fluorouracil 5% 21% • Irinotecan 5% 21% • Oxaliplatin NA 21% • BV 0% 12% DOSE REDUCTIONS TREATMENT DELAYS Supportive Therapies during INDUCTION TX FOLFIRI + BV FOLFOXIRI + BV 74 pts 76 pts G-CSF* 15% 26% ESA** 3% 7% LMWH*** 11% 8% Oral Anticoagulant 0% 0% *G-CSF, Granulocyte-Colony Stimulating Factor **ESA, Erithropoiesis-Stimulating Agents ***LMWH, Low Molecular Weight Heparin Maximum Per Patient Toxicities during MAINTENANCE TX FOLFIRI + BV 74 pts FOLFOXIRI + BV 76 pts G1-2 G3-4 G1-2 G3-4 Vomiting 9% 0% 1% 0% Diarrhea 9% 0% 7% 0% Stomatitis 11% 0% 11% 0% Hand-Foot Syndrome 7% 0% 3% 0% Neutropenia 0% 0% 7% 0% Hypertension 8% 1% 8% 0% Proteinuria 3% 0% 5% 0% Venous thrombosis 0% 0% 1% 4% Bleeding 9% 0% 8% 0% Conclusions The study is still ongoing Accrual updated at May 31st 2010 is 272 patients These preliminary results demonstrate that both treatment arms are safe and feasible The side-effects occur with the expected incidence and there were not unexpected toxicities Enrolling Centers Ancona S. Cascinu, M. Scartozzi, R. Berardi Monza P. Bidoli, R. Longarini, D. Cortinovis Arezzo S. Bracarda, M. Sisani, S. Del Buono Napoli – Federico II° G. Tortora, C. Carlomagno, A. De Stefano Aviano S. Frustaci, A. Buonadonna, G. Tabaro Padova S. Lonardi, A. Cappetta Brescia A. Zaniboni, M. Mazzocchi Parma Caltanissetta S. Vitello, C. Raimondi Pisa A. Ardizzoni, R. Camisa, E. Rapacchi, F. Pucci, F. Leonardi A. Falcone, G. Masi, F. Loupakis, E. Vasile, I. Brunetti Cremona R. Passalacqua, M. Dalla Chiesa, G. Tomasello, S. Lazzarelli Pistoia M. Di Lieto Cuneo M. Merlano, C. Granetto, M. Gasco Pontedera G. Allegrini, L. Marcucci, S. Lucchesi Firenze L. Fioretto, A. Ribecco, F. Martella Prato A. Di Leo, A. Ciarlo, F. Del Monte Genova Galliera A. De Censi Reggio Emilia C. Boni, M. Banzi, R. Gnoni Genova IST S. Chiara, C. Sonaglio, D. Garbarino Roma CBM Lecce V. Lo Russo, L. Petrucelli Roma - Gemelli Livorno F. Cappuzzo, S. Cupini, Dr. C. Barbara, V. Safina, A. Antonuzzo Roma - Umberto I° G. Tonini, D. Santini, B. Vincenzi, O. Venditti C. Barone, Dr. P. Di Nardo, Dr. A. Inno, Dr. A. Amoruso E. Cortesi, A. Tuzi, P. Trenta, A. Pellegrino, M. Mazzoli Milano HSR E. Villa, M. Ronzoni, V. Ricci Sondrio A. Bertolini, E. Menatti Milano Niguarda S. Siena, A. Sartore-Bianchi, Bencardino, Y. Franzosi Mirano O. Vinante, B. Silvestri K. Torino Viareggio L. Ciuffreda, P. Racca, C. Bonfadini, C. Taverniti D. Amoroso, C. Valsuani, M. Ricasoli, C. Puccetti
Scarica