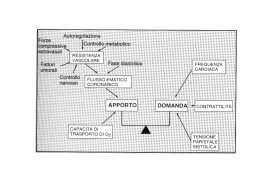
CORSO DI CERTIFICAZIONE DI COMPETENZA in ECOGRAFIA VASCOLARE GENERALE Lezione 2 Studio ecografico dell’aterosclerosi pre-clinica:spessore mio-intimale e funzione endoteliale Settore formazione 2007-2009: Direttore: Paolo G. Pino Marco Campana, Antonella Moreo, Fausto Rigo, Ketty Savino ATEROSCLEROSI Recenti scoperte Condizioni morfofunzionali che precedono il restringimento del vaso e l’inizio dei sintomi: • DISFUNZIONE ENDOTELIALE • INFIAMMAZIONE Carattezzazione Placca • CALCIFICAZIONE • Ossidazione lipoproteine Precoci modificazioni molecolari e cellulari del processo aterogenetico • Adesione monociti • Formazione Foam cells • Ispessimento parietale Ecografia vascolare • A causa del remodeling della tunica media lo sviluppo iniziale della placca aterosclerotica non è accompagnato da una riduzione del lume vascolare. • In questa fase non sono osservabili modificazioni angiografiche, mentre l’Ecografia è in grado di visualizzare le alterazioni morfo-funzionali della parete arteriosa Dipartimento CardioCardio-Toracico Università di Pisa METODI DI VALUTAZIONE ANATOMICA - ECOGRAFIA TRANSCUTANEA (arterie carotidi) VALUTAZIONE SMI - ULTRASONOGRAFIA INTRAVSCOLARE (arterie periferiche) SPESSORE INTIMALE monocita Danno e disfunzione endoteliale cell. schiumosa Espressione molecole I macrofagi fagocitano Migrazione e di adesione, adesione ox-LDL attraverso proliferazione miociti migrazione monociti scavenger receptor Placca ateromasica SPESSORE MEDIOMEDIO-INTIMALE CAROTIDEO DEFINIZIONE • Spessore del complesso intima intima--media della parete carotidea • Misurabile come distanza tra l’interfaccia sangue sangue-intima e l’interfaccia mediamedia-avventizia Dip. CardioCardio-Toracico - Università di Pisa IMPORTANZA CLINICA DELLO SPESSORE MEDIO-INTIMALE CAROTIDEO • Marker di aterosclerosi periferica • Marker di aterosclerosi coronarica • Studio dell’efficacia degli interventi terapeutici Dipartimento CardioCardio-Toracico - Università di Pisa VALUTAZIONE DELL’IMT ANATOMIA PA ECOGRAFIA Avventizia Media Intima Lume vascolare PP Intima Media Avventizia Dipartimento CardioCardio-Toracico – Università di Pisa “IMT” misura non valida “IMT” misura valida INTIMA-MEDIA THICKNESS METHODS OF MEASUREMENT: MANUAL CURSOR PLACEMENT INTIMA-MEDIA THICKNESS METHODS OF MEASUREMENT: AUTOMATED COMPUTERIZED EDGE-DETECTION INTIMA-MEDIA THICKNESS METHODS OF MEASUREMENT The three most frequently used measurements in clinical trials are as follows: • Mean of the maximum IMT of the 4 far walls of the carotid bifurcations and distal common carotid arteries (CBM max) • Mean maximum thickness (M max) of up to 12 different sites (right and left, near and far walls, distal common, bifurcation and proximal internal carotid) • Overall single maximum IMT (T max) Dipartimento CardioCardio-Toracico - Università di Pisa Doppler TSA- IMT • Misurare IMT sulla parete posteriore della carotide comune ad 1 cm dalla biforcazione in un segmento di carotide di circa 1 cm, prendendo almeno 2- 3 proiezioni (valore medio o massimo) • immagini “zoomate” • misurazioni ripetute o operatori indipendenti • segnare le misure IMT delle 2 CC separatamente • segnalare se valore medio o massimo SPESSORE MEDIO-INTIMALE CAROTIDEO METODI DI CALCOLO RIPRODUCIBILITA’ DATI variabilita’ intra ed interosservatore ? Dipartimento CardioCardio-Toracico - Università di Pisa Complesso intima-media Correlazione con fattori di rischio CV Età, familiarità per malattie CV Fumo Diabete, sindrome metabolica & insulino-resistenza Ipertensione arteriosa, ipertrofia ventricolare sin Dislipidemie ( LDLc, trigliceridi, LP(a), HDLc) Fattori emocoagulativi ( PAI1, tPA e D-Dimero, Viscosità plasmatica, WWF, fibrinog., VIIIc) • Omocisteina • Nuovi FDR (CMV, Clamidia, parodontopatie, livelli di antiossidanti, D allele dell’ACE, sideremia e ferritina)... • • • • • • Complesso intima-media Correlazione con score riassuntivo dei fattori di rischio CV 12 6 SMARTscore 9 R = 0,719 p < 0,0001 3 0,2 0 0,4 0,6 0,8 10 Common carotid IMT (mm) Lupi, ESC 2002 La diagnosi precoce di aterosclerosi coronarica - Torino 20/11/2004 1,2 Complesso intima-media Correlazione con AS coronarica Anderson, JACC 1995 La diagnosi precoce di aterosclerosi coronarica - Torino 20/11/2004 Complesso intima-media Correlazione con malattia AS vascolare (ARIC study) P<0.01 Burke, Stroke 1995 Complesso intima-media Correlazione con prognosi (CH Study) p<0.01 vs 1t Quintile O’Leary, ’Leary, NEJM 1999 Complesso intima-media Correlazione con prognosi (CH Study) Crouse, Circulation 2003 Complesso intima-media End-point surrogati e studi di intervento farmacologico p<0.05 vs Pravastatina Taylor, Circulation 2002 (ARBITER study) Lo Studio della Funzione Endoteliale L’ENDOTELIO NELLA PATOLOGIA CARDIOVASCOLARE “ ENDOTHELIAL CELLS…(ARE)…MORE THAN A SHEAT OF NUCLEATED CELLOPHANE” LORD FLOREY, 1966 RUOLO CENTRALE NELLA REGOLAZIONE DELL’OMEOSTASI CARDIOCIRCOLATORIA 1998 • TONO VASCOLARE • ADESIONE E AGGREGAZIONE PIASTRINICA • COAGULAZIONE LOCALE • CRESCITA VASCOLARE • INFIAMMAZIONE Malattie Cardiovascolari e Disfunzione Endoteliale Aterosclerosi Scompenso cardiaco Vasospasmo Danno da riperfusione Trombosi Iperlipidemia DISFUNZIONE ENDOTELIALE Angiopatia diabetica Reazioni immuni Riocclusione Infiammazione Ipertensione Arteriopatie obliteranti periferiche Dipartimento Cardio Toracico – Università di Pisa How is endothelial function assessed ? FISIOLOGIA DELL’ENDOTELIO SANGUE CELLULE • PMN • Monociti • Piastrine ENDOTELIO MUSCOLATURA LISCIA VASCOLARE FORZE ELASTICHE • Shear stress • Pressione SOSTANZE VASOATTIVE • Acetilcolina • Peptidi ( trombina, sostanza P, vasopressina) • Chinine (bradichinina) • Amine (serotonina) • Nucleotidi (ATP; ADP) • Metaboliti (leucotriene C4) “FATTORI DI DERIVAZIONE ENDOTELIALI” rilasciamento contrazione proliferazione Dipartimento Cardio Toracico – Università di Pisa PRINCIPALI MECCANISMI INTRACELLULARI MEDIANTI L’AZIONE DELL’NO SHEAR STRESS BRADICHININA Ach M CELLULA ENDOTELIALE L-Arg → R-NO NO CELLULA MUSCOLARE LISCIA ? GC GTP → cGMP K+ Ca++ ? G-Kinasi Ca++/Mg++ ATPasi Ca++ VASODILATAZIONE EFFETTI VASOPROTETTORI DELL’ NO • Vasodilatazione (attraverso rilasciamento della cellule della muscolatura liscia) • Inibizione della crescita (attraverso azioni sulla cellula della muscolatura liscia) • Inibizione dell’adesione/aggregazione piastrinica • Inibizione delle interazioni endotelio/leucociti • Controbilancia l’effetti dell’anione superossido? Dip. Cardio-Toracico - Università di Pisa ASSESSMENT OF ENDOTHELIAL FUNCTION IN HUMANS STUDY OF VASCULAR REACTIVITY STUDY OF VASCULAR REACTVITY • • • • MICROCIRCULATION: CORONARY CUTANEOUS MUSCLE • MACROCIRCULATION: - EPICARDIAL ARTERIES - BRACHIAL, RADIAL, FEMORAL ARTERIES VALUTAZIONE CLINICA DELL’ENDOTELIO MACROCIRCOLO CORONARIE ART.PERIFERICHE (art.radiale,art.femorale ANGIOGRAFIA QUANTITATIVA + IVUS ULTRASONOGRAFIA NON INVASIVA (ECO--DOPPLER TRANSCUTANEO) (ECO Dipartimento Cardio Toracico – Università di Pisa FLOW (Q) Endothelium SHEAR STRESS (ττ) = 4µQ πR2 ENDOTHELIUM-INDEPENDENT STIMULI • NITRATES: SODIUM NITROPRUSSIDE, NITROGLYCERIN • DIRECT VASODILATORS: PAPAVERINE, ADENOSINE (?) NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY Technique • Subject preparation • Equipment: high resolution ultrasound with broad-band ( 7 to 12 Mhz) linear array transducers • Image acquisition : 2D gray-scale imaging, Stereotactic probeholding device NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY FMD endothelium-dependent TIMING OF FMD Sinoway et al. Circ Res 1989 STIMULUS: REACTIVE HYPEREMIA BASELINE AFTER ISCHEMIA Flow velocity (Doppler) Reactive hyperemia is calculated as maximal per cent flow increment above baseline after ischemia. Arterial flow: flow velocity x heart rate x vessel area (π πr2). NO IS RESPONSIBLE FOR FMD OF HUMAN PERIPHERAL CONDUIT ARTERIES IN VIVO • JOANNIDES R CIRCULATION 1995 • LIEBERMAN Am J Cardiol 1996 FMD following wrist and upper arm occlusion in humans: the contribution of NO Doshi S Clinical Science 2001 • Dilatation following upper arm occlusion is greater than that observed after wrist occlusion. • L-NMMA infusion revealed that FMD following upper arm occlusion is substantial component not mediated by NO, most probably related to tissue ischaemia around the brachial artery. NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY FMD endothelium-independent: NTG NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY Analysis: Anatomic landmarks 1. Caliper measurement 2. Computerized measurement CALIPER MEASUREMENT (manual) OF FMD baseline: 0.349 cm diam eter (cm ) BASELINE -360 -300 -240 -180 -120 cuff inflation • • • • • 60 s: 0.373 cm FMD = 6.9% 0.380 AFTER REACTIVE HYPEREMIA 0.360 0.340 -60 0 TIME (seconds) 60 120 180 cuff deflation 40 HEALTHY SUBJECTS (21-51 YEARS) 4 MEASUREMENTS (BASELINE, 1-2 DAYS, 1-2 WEEKS, 2-4 MONTHS) FMD 7±1% (RANGE 0-17%) REPRODUCIBILITY (INTEROBSERVER VARIABILITY): 1.2±0.4 (17%) VARIATION COEFFICIENT AMONG DIFFERENT MEASUREMENTS: 1.8 (25%) SORENSEN KE ET AL. BR HEART J 1995 COMPUTERIZED MEASUREMENT edge-detection software system ENDOTHELIUM-DEPENDENT RESPONSE % of diameter 10 8 6 flow velocity by * doppler 4 2 0 -360 -300 -240 -180 -120 -60 -2 0 -4 ISCHEMIA * * FMD max FMD 60 s FMD AUC 60 120 180 seconds NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY Validation and Relevance of The Method CALIPER MEASUREMENT (manual) OF FMD 40 healthy subjects (21-51 years) 4 measurements (baseline, 1-2 days, 1-2 weeks, 2-4 months) • • fmd 7±1% (range 0-17%) reproducibility (interobserver variability): 1.2±0.4 (17%) • var. coeff. : 1.8 (25%) Sorensen ke et al. br heart j 1995 COMPUTERIZED MEASUREMENT 40 healthy subjects (26-56 years) 2 measurements in the same day • max FMD (56 sec) 6.5±2.9% Var. Coeff: 10% • FMD (60 sec) 4.2±2.5% Var. Coeff: 18 % • FMD AUC (56 sec) 525±260% Var. Coeff: 21 % • max FMD, FMD 60 sec e FMD AUC are significantly related (r=0.75-0.82) Beux F Ultrasound Med Biol 2001 CLINICAL EVALUATION OF ENDOTHELIUM Flow- mediated vasodilation in patients with CAD 10 Brachial artery 9 diameter 8 (% change) 7 Normal CAD * * p < 0.05 6 5 * 4 3 2 1 0 Reactive hyperemia Nitroglycerin E. H. Lieberman Am. J. of Cardiol.1996 NON INVASIVE EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY Validation and Relevance of The Method CLOSE RELATION OF ENDOTHELIAL FUNCTION IN THE HUMAN CORONARY AND PERIPHERAL CIRCULATIONS 18 16 BRACHIAL ARTERY DIAMETER ( % change) REACTIVE HYPEREMIA 14 12 10 8 6 (n= 26) (n=11) (n=7) * * * 4 2 0 (n= 26) * P = 0.08 ** P < 0.001 CAD (angio) and Coronary Endothelial Dysfunction (n=11) No CAD(angio) and Coronary Endothelial Dysfunction (n=7) No CAD (angio) and Normal Coronary Endothelial function T. Anderson et al. JACC 1995 Ultrasound Study Early Disease • Asymptomatic Children and young adults with RF for ATS- Lancet 1992 • Hypercolesterolemia in Children-J Clin Invest 1994 • Active Smoking- Circul. 1993 • Passive Smoking-EHJ • Diabete Mellitus JACC 1996 • Hyperhomocisteinemia- Circul 1997 Studies of Reversibility • Antioxidant Vit.C in CADCircul.1996 • L-arginina in Hypercholest.-J Clin Invest • Estrogen Therapy- Clin Endocr. EVALUATION OF ENDOTHELIAL FUNCTION IN THE BRACHIAL ARTERY ADVANTAGES • non invasive procedure • large repeatibility over the time • correlation with coronary circulation • correlation with clinical end-points DISADVANTAGES • reproducibility • low degree of response→ → large number of subjects to study • limited possibility to assess mechanisms European Heart Journal (2005) 26, 363–368 GUIDELINES FOR THE ULTRASOUND ASSESEMENT OF ENDOTHELIAL DEPENDENT FMD OF BRACHIAL ARTERY JACC 2002 Ruolo della disfunzione endoteliale nella stratificazione del rischio cardiovascolare LongLong-Term FollowFollow-Up of Patients With Mild Coronary Artery Disease and Endothelial Dysfunction Suwaidi J, Circulation. 2000;101:948 FollowFollow-up (average 28 month; month; 11 to 52 months) was obtained in 157 patients with mildly diseased coronary arteries (angiographically coronary artery lesions <40% 40% lumen diameter stenosis without evidence of coronary spasm) Coronary vascular reactivity evaluation: evaluation: graded administration of intracoronary acetylcholine, adenosine, and nitroglycerin and intracoronary ultrasound at the time of diagnostic study Patients were divided on the basis of their response to acetylcholine into 3 groups: groups: group 1 (n=83 (n=83), 83), patients with normal endothelial function; function; group 2 (n=32 (n=32), 32), patients with mild endothelial dysfunction; dysfunction; and group 3 (n=42 (n=42), 42), patients with severe endothelial dysfunction. dysfunction. • % Change CBF (Ach) • 200 150 100 50 0 -50 174 P<0.001 * 24 * -38 Group 1 Group 2 CBF: Volumetric coronary blood flow; Normal coronary endothelium: CBF of >50%; mild: CBF between 0% to 50%; severe: percent change in CBF <0%. † 15 Group 3 % Cardiac events • 14 10 5 0 P<0.05 0 Group 1 0 Group 2 Group 3 LongLong-Term FollowFollow-Up of Patients With Mild Coronary Artery Disease and Endothelial Dysfunction Suwaidi J, Circulation. 2000;101:948 September 1995 ECG of 5858-yearyear-old patient at time of endothelial function evaluation (September 7, 1995). Mean percent change in CBF in response to acetylcholine was -35%. July, 1997 B, ECG when patient presented with 3 hours of typical anginal pain and elevated creatine kinase to 800 U (July 6,1997), revealing new TT-wave inversion in anterolateral leads. LongLong-Term FollowFollow-Up of Patients With Mild Coronary Artery Disease and Endothelial Dysfunction Suwaidi J, Circulation. 2000;101:948 A, Coronary angiogram (left coronary artery in left cranial view) of 5151-yearyearold patient at time of endothelial function evaluation (January 11, 11, 1996), 20% diameter 1996), demonstrating 20% stenosis in midmid-LAD (arrow). (arrow). Mean percent change in CBF in response to acetylcholine was -50% 50%. B, Patient who presented on August 1, 1997, 1997, with progressive exertional angina and dyspnea. dyspnea. Exercise sestamibi revealed large, reversible anterolateral perfusion defect, defect, and repeated coronary angiography revealed 95% 95% diameter stenosis in midmid-LAD (arrow). (arrow). Patient successfully underwent percutaneous coronary angioplasty and stent placement with resolution of symptoms. symptoms. January 1996 Aug. 1997 Peripheral vascular endothelial function testing as a noninvasive indicator of coronary artery disease • Subjects with CAD by ExMPI (n = 23) 23) had a lower FMD (6.3 ± 0.7%) than those without CAD by ExMPI (n = 71) 71) (10. 10.5 ± 0.6%; P = 0.0004) 0004). • Flowdilation was highly Flow-mediated predictive for CAD with an odds ratio of 1.32 for each percent decrease in FMD (p = 0.001) 001). • TwentyTwenty-one of 23 subjects who were positive for ExMPI had an FMD <10% 10% (sensitivity 91% 91%), whereas only two of 40 subjects with an FMD 10% 10% were ExMPIExMPIpositive (negative predictive value: value: 95% 95%). • Individuals with an FMD <10% 10% exercised for a shorter duration than those with an FMD 10% 10% (456 ± 24 vs. vs. 544 ± 31 s, respectively; respectively; P = 0.02) 02). (ExMPI) Kuvin JT, JACC Vol.38,7 2001:1843 Impaired Flow-Mediated Dilation and Risk of Restenosis in Patients Undergoing Coronary Stent Implantation • Was studied 136 patients with single-vessel CAD undergoing percutaneous coronary intervention (PCI) with stenting and at least 6 months of follow-up. • All patients underwent ultrasound detection of brachial artery reactivity 30 days after PCI Risk Stratification for Postoperative Cardiovascular Events via Noninvasive Assessment of Endothelial Function Gokce N, Circulation. 2002;105:1567-1572 • • Was preoperatively examined brachial artery vasodilation using ultrasound in 187 patients undergoing vascular surgery. surgery. Patients were prospectively followed for 30 days and 1.2 years after surgery FortyForty-five patients had a postoperative event, including cardiac death (3), myocardial infarction (12), 12), unstable angina/ischemic ventricular fibrillation (2), stroke (3), or elevated troponin I, reflecting myocardial necrosis (25) 25). • Preoperative endotheliumendothelium-dependent FMD was significantly lower in patients with an event (4.9±3.1%) than in those without an event (7.3±5%; P<0.001), 001), whereas endotheliumendothelium-independent vasodilation to nitroglycerin was similar in both groups. groups. • When a flowflow-mediated dilation cutpoint of 8.1% was used, endothelial function had a sensitivity of 95% 95%, specificity of 37% 37%, and negative predictive value of 98% 98% for events. events. High (>8.1%) High (>8.1%) Middle (4.2– (4.2–8.1%) Low tertile (<4.2%) Middle (4.2– (4.2–8.1%) Low tertile (<4.2%) Endothelial Dysfunction and Cardiovascular Risk Prediction in Peripheral Arterial Disease Additive Value of FMD to Ankle-BrachialPressure Index FMD > median • 131 patients monitored for a mean of 23 ±10 months. months. • 18 had a coronary event, cerebrovascular event, and peripheral event. event. • The median FMD was lower in patients with an event than in those without (5.8% versus 7.6%, P0.05) 05) • The cardiovascular event rate was higher in patients with FMD below the median versus those with FMD above the median (P0.001) 001). • BelowBelow-median ABPI and FMD combined was more accurate in predicting risk Brevetti G, Circulation. 2003; 108:2093 12 9 a a FMD < median Prognostic Role of Reversible Endothelial Dysfunction in Hypertensive Postmenopausal Women • A total of 400 consecutive postmenopausal women with mildhypertension mild-toto-moderate and impaired FMD underwent ultrasonography of the brachial artery at baseline and after six months, while optimal control of blood pressure was achieved using antihypertensive therapy. therapy. • They were then followed up for a mean period of 67 months (range 57 to 78) 78). Modena M.G. J Am Coll Cardiol 2002;40:505 CONCLUSIONI Lo funzione endoteliale rappresenta un marker della “salute” vascolare e gioca un ruolo importante nella patogenesi e nella prognosi delle malattie cardiovascolari. Lo studio della funzione endoteliale rappresenta un valido strumento clinico. La mancanza di una procedura standardizzata dello studio della funzione endoteliale ne limitano a tutt’oggi l’impiego nella pratica clinica quotidiana. Dipartimento Cardio Toracico – Università di Pisa
Scarica