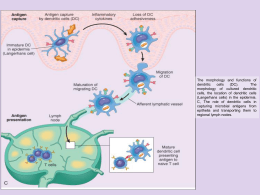
Tolleranza delle cellule T nei tessuti linfoidi periferici Vigorous reactivity against pathogens A lack of overt reactivity to self Both are best achieved when lymphocytes express diverse, clonally distributed antigen specific receptors (clonal selection theory) As the organism cannot predict the precise pathogen-derived antigens that will be encountered, the immune system relies on the generation and maintenance of a diverse T-cell receptor (TCR) repertoire GOD, generation of immune-receptor diversity Concept of Immune Regulation • Immune responses are tightly regulated by complex interactions of cells & mediators, and by mechanisms to prevent anti-self reactivity • Failure of regulatory control can occur… – Enhancement of immune responses or infection can generate autoimmune reactions (loss of self–tolerance) – Decrease of immune responses may lead to an immunodeficiency state – Shift in immune responses can lead to allergy Immunological Tolerance History - Ehrlich, Owen, Burnet - Billingham, Brent and Medawar Owen’s observation 1945 Burnet’s Clonal Selection Model: Central Tolerance DEVELOPMENT MATURITY Clonal Deletion Anti-self Self Ag Lymphocyte Differentiation Anti-non-self Lymphocyte Activation Foreign Ag Burnet postulated that there was a temporal window of tolerance such that antigens encountered while the immune system was immature tolerized the relevant lymphocytes. Medawar’s experiment demonstrating neonatal tolerance induction (Nobel Prize) Medewar subsequently investigated the effects of transferring hemopoietic cells from histoincompatible mice at different times after birth. He found that if the cells were transferred in the first few days of life (but not later) the recipient mouse acquired lifelong tolerance to the antigens of the donor. Immunological Tolerance • Definition and Properties – Specific unresponsive state induced by exposure to antigenic epitopes – Tolerance to self is initially induced during embryonic life, and is maintained by antigen – Tolerance occurs in both T and B cells – Multiple mechanisms of tolerance exist Tolerance • Central Tolerance - this occurs during lymphocyte development. • Peripheral Tolerance - occurs after lymphocytes leave the primary lymphoid organs. Central Tolerance The thymus provides a fundamental initial step for the elimination of potentially dangerous self-specific T cells Peripheral tolerance Acquisition and maintenance of peripheral tolerance Different hypotheses: •Self-nonself discrimination (Bretscher, Cohn) •INS model (Janeway) •Danger model (Matzinger) •Localization dose and time model (Zinkernagel) Self nonself Bretscher: two step, two-signal model Signal two is given by a T cell Cohn: associative recognition of antigen Infectious nonself and non-infectious self model No peripheral tolerance only central tolerance Recognition of a pathogen by PRRs induces a set of endogenous signals, including costimulatory molecules (B7), inflammatory and effector cytokines, and CD1d molecules. Additionally, some cells can phagocytose the pathogen (not shown), process its protein constituents, and present its peptides to T cells. Recognition of peptides derived from a pathogen, along with costimulatory molecules induced by the pathogen, results in T cell activation. Effector cytokines induced by the pathogen instruct the activated T cells to differentiate into a particular effector cell type (T1 or T2). Activated T cells then deliver an inducible signal (usually a member of the TNF family, such as CD40L or FasL) to the target cell in an antigen-specific manner: the target cells of T1 and T2 being macrophages and B cells, respectively. L, ligand. Danger model Danger model Absence of signal two induces tolerance Danger Model Anti-DEC205 Steady state DC Come viene indotta la toleranza allo steady state? Topi transgenici esprimenti OVA sotto il cotrollo di RIP Localization dose and time model Localization dose and time model TCR tg anti-gp33 x RIP-gp33 ignoranza 20 30 50 40 30 20 10 0 60 20 0 0 10 20 30 100 80 60 40 20 0,1 Bpep mg/ml 1,0 CD44 10 30 10 20 30 40 high frequency IFNg production 80 70 60 50 40 30 20 10 0 0,0 0,01 Transient peptide presentation by B cells 40 CD69 0 Days low frequency 40 20 CD69 upregulation % CD69 high % TCR high TCR downregulation 120 0,01 e CD25 BALB/c 0,0 40 Anti-IgG2ab TCR transgenic mice IFNg ng/ml % of CD25+ 100 10 100 80 60 40 20 0 0 % of CD69+ 0 0 c proliferation 50 40 30 20 10 0 % of CD44high %Vb14+ on CD4+ Localization dose and time model 0,1 Bpep mg/ml 1,0 8 7 6 5 4 3 2 1 0 naive High frequency Low frequency 0 10-5 10-4 10-3 10-2 Bpep mg/ml 10-1 1 Chronic peptide presentation by B cells Organi immunoprivilegiati Nel 1989 sono stati isolati anticorpi monoclonali citolitici per diverse linee cellulari La proteina riconosciuta da questi anticorpi è stata denominata FAS L’espressione costitutiva di FAS in trasfettanti porta alla morte cellulare in seguito ad incubazione con anticorpi antiFAS FAS trasduce un segnale apoptotico FAS espresso in : TIMO, FEGATO, CUORE, POLMONI, RENI, OVAIO Timo: FAS espresso in tutte le popolazioni ma non nei doppi negativi Periferia: FAS espresso nei T maturi attivati FASL: 40000 D, induce morte cellulare se interagisce con linee cellulari esprimenti FAS FASL: espresso dalle cellule T attivate, espresso nel TESTICOLO, CORNEA, TIMO (organi immunoprivilegiati) FASL esiste anche solubile in forma trimerica Per indurre morte cellulare è necessario il cross-linking di FAS Gli organi immunoprivilegiati esprimono il ligando di FAS Se cellule T attivate arrivano agli organi immunoprivilegiati sono uccise mediante interazione FAS-FASL Dimostrato direttamente per la cornea Walker and Abbas 2002, 2 Walker and Abbas 2002, 2 Tolerance and Regulatory T cells Patrolling and Keeping the periphery in check. • Regulatory T cells patrol periphery and maintain tolerance : • Self-reactive T cells are under the constant control of regulatory T cells. • Variety of regulatory or “suppressor” T cells: • Late 70’s - Early 80’s Present Regulatory T Cells • CD25+CD4+ thymic origin • Th3 - Induced by oral feeding of antigen • TGF-b1 producing (IL-10). • TGF-b1 dependent • Tr1 - Induced • Antigen administration in the presence of IL-10 • IL-10 dependent • All induced by Ag X, thus known specificity. Tregs The reincarnation of the suppressor T cell Number of publications More questions than answers. n 1 * Questions ? 1995 - Present Answers CD4+CD25+ immunoregulatory T cells The rebirth and revival…mid 1990’s. Naturally-occurring or “professional” regulatory T cells. Immunosuppressive in vivo : • • Day 3 thymectomy Depletion of CD4+CD25+ T cells Irradiation Gastritis, oophritis, orchitis, thyroiditis, pancreatitis, colitis Co-transfer with CD4+CD25- T cells suppresses autoimmune disease. Absence of CD4+CD25+ T cells Increased immunoreactivity to antigens. CD4+CD25+ regulatory T cells General characteristics Secondary lymphoid tissues Originate from thymus. Role of periphery ? “Partially activated” phenotype : 5-10% CD4 Unique lineage of CD25+ (IL-2R) T cells No other marker for regulatory T cells. Altered negative selection? TCR specificity is unknown : CD25 Differ from conventional, activated CD25+ T cell. Thymic developmental pathway is unclear: CD62Lhigh, CD69low, CTLA-4, GITR and CD45Rblow Diverse T cell repertoire. Self-specific Cross-reactive to foreign? Hyporesponsive (anergic) : Unresponsive to TCR stimulation : restored by IL-2. Do not produce IL-2. T cell activation induces expression of functional T cell surface molecules MHC/peptide Activated CD4+ T cell CD40L TCR APC TCR Resting CD4+ T cell CD25 CD69 CD44 CD25 is not a marker of Treg after T cell activation. Only in the naïve T cell repertoire. CD4+CD25+ regulatory T cells suppress T cell proliferation and cytokine production Proliferation Cytokine Production 77.6 CD4+ CD8+ and T cells IL-2 CD8+ 69 CD8+ / CD4+CD25+ CD25 Suppress the induction of IL-2 mRNA # CD4+CD25- ( ) or CD4+CD25+ ( ) T cells IFN-g IFN-g (ng/ml) CPM IL-2 CD8+ CD8+/- CD8+/+ CD4+CD25+ CELLS REQUIRE ACTIVATION TCR ENGAGEMENT FOR Treg ACIVITY DO11.10 CD4+ Tg WT CD4+CD25+ CD4+CD25+ T cell mediated suppression Unknown mechanism. • • • • • CD4+CD25+ T cells inhibit the IL-2/IL-2R system in T cells Do not suppress by consuming IL-2. Suppressor molecules are not defined. Not directly cytolytic. Cell-contact dependent and cytokine independent. Treg effector functions CD4+CD25+ mediated suppression Requirement for a T:T cell interaction APC CD4+ CD25+ CD8+ Activation CD4+ CD25+ Suppression CD8+ Direct evidence for T:T conjugates ? Role for cytokines? CD4+ CD25+ X T cell Responder IL-10 & TGF-b1 Immunosuppressive effects on APC and T cells But the role of differentiated Tregs is not abrogated by inhibiting IL-10 and TGF-b1 Tissue-specific CD4+CD25+ mediated disease protection in the absence of IL-10. CD4+CD25CD4+CD25+ CD4+CD25- CD4+CD25IL-10-/- CD4+CD25+ Nude Gastritis IBD No Gastritis No IBD No Gastritis IBD develops ! Altered peptide ligands o peptidi antagonisti
Scarica