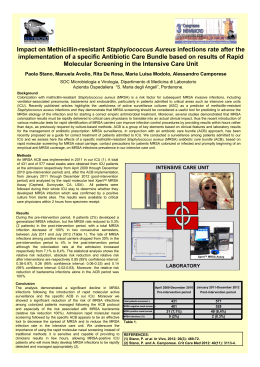
Resistenze batteriche e terapia delle infezioni postoperatorie Fausto de Lalla,Vicenza Postoperative infection 2006 Despite the great advances in surgical technique and antibiotic prophylaxis, and ongoing research in this field, wound infection remains a considerable cause of morbidity and mortality among surgical patients Antibiotic Resistance The knowledge of sensitivity patterns of the most likely etiological agents of postoperative infections is pivotal for the success of both - perioperative prophylaxis, and - empiric treatment of SSIs TRADITIONAL CLASSIFICATION Clean surgery Clean-contaminated surgery Contaminated surgery Dirty surgery Pathogens Causing Surgical Site Infections Are different, in respect to the surgical procedure and the site of infection. Infections following: - CLEAN SURGICAL PROCEDURES (with or without implantation of vascular grafts or prosthetic devices) - SUPERFICIAL,INCISIONAL SSIs (i.e. simple infection of the surgical incision, involving only skin and subcutaneous tissue) : are most often caused by Staph. aureus or coag. negative staphylococci (patient’s skin flora, surgical team, exogenous environment) Pathogens Causing Surgical Site Infections Deep and “organ space” infections following CLEAN- CONTAMINATED SURGERY : - are more often polymicrobial infections - are caused by the normal endogenous microflora of the structure which has been transected Most Likely SSI Pathogens according to Operation Type Operation Appendectomy colorectal Gastroduodenal Biliary tract OB/GYN. Urologic Head and neck negative Likely pathogens - gram-negativi bacilli + anaerobes (B.fragilis) - gram-negativi bacilli oropharingeal anarobes; streptococci - gram-negativi bacilli±Enterococcus spp - gram-negativi bacilli + anaerobes (B. fragilis)± enterococcus spp; streptococc - gram-negative bacilli - oropharingeal anarobes ± grambacilli; streptococci; Eziologia delle infezioni postoperatorie -Resistenze -gram positivi - gram negativi - microrganismi in situazioni particolari Emerging Gram-positive Microorganisms in Postoperative Infections MR staphylococci VR enterococci Surgical Infection with Antibiotic-resistant Microorganisms Surgical patients with infections by MR staphylococci or VRE have: a significantly higher mortality rate longer hospitalization longer treatment before the discharge than patients with infections by MS staphylococci or glycopeptide sensitive enterococci Nichols RL, Am J Med 1998; Gleason et al, Arch Surg 1999; Mekontso DA, et al. CID 2001; Edmond MB, et al. CID 1996 Significance of Enterococci in Surgical Infections Enterococcal bacteremia carries a serious prognosis Patients with intra-abdominal infection and an initial isolation of enterococci have a significant higher treatment failure rate * VRE infections, and particularly VRE bacteremia, are associated with high morbidity and mortality** * Burnett RJ, Dellinger EP, et al. Surgery 1995 ** Edmond MB, et al. CID 1996 Microbiologia delle peritoniti secondaria(comunitaria) e postoperatoria (ospedaliera) microrganismo comunitaria (%) ospedaliera(%) - Enterococchi E. coli Enterobacter spp. Bacteroides spp Klebsiella spp S.aureus S.coagulasi neg. Streptococcus spp Pseudomonas spp - Roehrborn A. CID 2001;33:1513-9 - - 5 36 3 10 7 1 1 14 2 21 19 12 7 7 6 5 4 6 p 0,001 0,005 0,05 NS NS 0,05 0,05 0,005 NS VRE: isolamenti per materiale ANNO 2001 2002 MATERIALE N° ISOLAMENTI Feci 24 Urine 7 Ferita chir. 3 Sangue 2 Liquor 1 Drenaggio bil. 1 Feci 85 Urine 3 Piaga decubito Bile 1 1 MR Staphylococci in Surgical Site Infections (S.Bortolo Hospital) Dept. S.aureus MR/ tot S.aureus (%) - Neurosurg. - Cardiosurg. - Orthoped. TOTAL 35/39 (89.7) 11/18 (61.1) 32/58 (55.2) 78/115 (67.8) de Lalla F. J Hosp Infect 2002 Coag. Neg. staph. MR/ tot. CNS (%) 18/26 (69.2) 11/15 (73.3) 12/18 (66.7) 41/59 (69.5) MR Staphylococci in Surgical Site Infections in Italy Ancona and Pesaro Hospitals (676 patients) * - MR S. aureus/total S.aureus = 104/191 (54%) - MR CNS/total CNS = 71/138 (51%) S.Bortolo Hospital,Vicenza ** - MR S. aureus/total S.aureus = 78/115 (67.8%) - MR CNS/total CNS = 41/59 (69.5) 86 orthopedic centers (2,013 isolates from SSIs following TH or TK arthroplasties) *** - MR S. aureus/total S.aureus = 212/463 (46%) - MR CNS/total CNS = 156/304 (51%) * Giacometti A et al. J Clin Microbiol 2000; de Lalla et al,J Hosp Infect 2002;*** Mini E et al, J Chemother 2001 Implications of Resistance for Selection of Antibiotics in Surgery (1) TREATMENT OF ESTABLISHED INFECTIONS: 1) SSIs following clean surgery: - the high frequency of MR staphylococci as causative agents should be kept in mind, AND glycopetides should be administered in the empiric treatment of the most serious of these infections (e.g. prosthetic infections) - PERIOPERATIVE PROPHYLAXIS: - The administration of glycopeptides as prophylactic agents in clean prosthetic major surgery is suggested by some Authors (at least for those cardiovascular and orthopedic Depts. in which the prevalence of MR staphylococci is considerably high) - prophylactic glycopeptides are in clinical practice extensively used If the proportion of postoperative S. aureus infection caused by MRSA (in major vascular and orthopedic surgical prostheses) were to rise to 20%, we would probably advise using vancomycin or teicoplanin as prophylactic agents in both of these areas. Adam P Fraise, J Antimicrob Chemother 1998; 42:287-289 Antibiotic of choice in clean surgery prophylaxis Vancomycin may be the agent of choice in certain clinical circumstances,such as a cluster of MRSA mediastinitis or incision infection due to MR coag.neg staphylococci. A threshold has not been scientifically defined that can support the decision to use vancomycin. The decision should involve local considerations. CDC Guidelines Clinical consequences and cost of limiting use of vancomycin for perioperative prophylaxis:example of coronary artery bypass surgery (CABS) * - - - - -to compare clinical results and cost-effectiveness of no prophylaxis, cefazolin and vancomycin in CABS -Decision-analytic models -Vancomycin resulted in 7% fewer surgical infections and 1% lower all-cause mortality and saved $ 117 per procedure,compared with cefazolin. -Cefazolin resulted in substantially fewer infections and deaths and lower costs than no prophylaxis -Data on vancomycin’s impact on resistance are needed to quantify……..the future long term-consequences to society * Zanetti,Goldie, Platt, Emerg Infect Dis 2001;820-7 Glycopeptides Are No More Effective than ß-Lactam Agents for Prevention of Surgical Site Infection after Cardiac Surgery: a Meta-analysis (Bolon et al,CID 2004) 7 trials published between 1988-2002 on 5,761 subjects Glycopeptide : vancomycin (4 studies) or teicoplanin (3 trials) Comparators: cefazolin (3),cefuroxime (1),ceftriaxone (1),fluc+tobra (1) Prevalence of MRSA: low (6 Blinded: No (5 trials), yes (2studies) trials), high (1 study) RESULTS : neither agent proved to be superior for prevention of occurrence of SSI (primary outcome at 30 days !!) In subanalyses: - ß-lactams were superior to glycopeptides for prevention of chest SSIs, and - glycopetides were superior for prevention of SSIs caused by MR gram + bacteria. Implications of Resistance for Selection of Antibiotics in Surgery (2) during treatment with 3rd gen cephalosporins enterococcal superinfection can occurs the use of 3rd gen ceph.s is an important risk factor for VRE colonization and infection in surgical patients * in the hospitals with high rates of VRE, limitation of 3rd gen ceph.s use, with an increase of penicillins -LI combinations, is followed by a significant decrease in the VRE infection ** Dahms RA et al, Arch Surg 1998; ** May AK, Shock 2000 Implications of Resistance for Selection of Antibiotics in Surgery (3) - The particular role of Enterococcus spp. as an etiological agent of tertiary peritonitis (hospital acquired peritonitis) should be kept in mind (use of extended spectrum penicillins and penicillin- LIs combinations in the treatment of abdominal and pelvic surgical infections) - Postoperative infections in patients who have been hospitalized for a prolonged period prior to surgery, and/or have received prior antibiotic treatment are more likely to involve antibiotic resistant Gram negative bacilli(ESBL producing Klebsiella pneumoniae, E.coli, C.freundi, E.cloacae, S. marcescens …..).: the possible administration of carbapenems should be kept in mind
Scarica