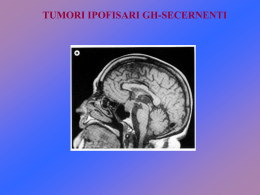
MALASSORBIMENTO, DISSENTERIA DIARREA ALTRE ENTEROCOLITI Seen here is a loop of bowel attached via the mesentery. Note the extent of the veins. Arteries run in the same location. Thus, there is an extensive anastomosing arterial blood supply to the bowel, making it more difficult to infarct. Also, the extensive venous drainage is incorporated into the portal venous system heading to the liver This is the normal appearance of terminal ileum. In the upper frame, note the ileocecal valve, and several darker oval Peyer's patches are present on the mucosa. In the lower frame, a Peyer's patch, which is a concentration of submucosal lymphoid tissue, is present. Note the folds are not as prominent here as in the jejunum This is the normal appearance of small intestinal mucosa with long villi that have occasional goblet cells. The villi provide a large area for digestion and absorption MALDIGESTIONE MALASSORBIMENTO BASI FISIOPATOLOGICHE L’intestino presenta un’enorme area superficiale, incrementata, a livello del tenue, dalla presenza dei microvilli (2 x 108/cm2). La motilità intestinale, parietale e degli stessi villi, consente l’intimo contatto tra parete intestinale e sostanze nutritizie e ne favorisce la progressione ed il trasporto nei linfatici. Alcuni processi digestivi si completano nella parete. La porzione prossimale dell’intestino tenue, normalmente è sterile per 1) acidità gastrica 2) peristalsi intestinale 3) produzione locale di Ig. Assorbimento differenziato Fe, Ca, vitamine liposolubili, grassi tenue prossimale Glucidi tenue prossimale e medio Aminoacidi tenue medio, ma anche altri tratti Sali biliari e vitamina B12 soprattutto tenue distale Acqua intestino crasso Maldigestione - Malassorbimento Alterato assorbimento di proteine, carboidrati, grassi, vitamine liposolubili ed altre vitamine, elettroliti, minerali, acqua, per alterazione di una o più delle seguenti funzioni digestive: digestione intraluminale digestione terminale (parietale) trasporto transepiteliale Diagnosi: in molti casi è necessaria la biopsia della mucosa intestinale Quadro anatomo-clinico Generale: calo ponderale, diminuzione di crescita, mucositi, edemi da ipoproteinemia Apparato gastroenterico: diarrea con feci abbondanti giallastre, grassose; metorismo; dolori addominali e senso di distensione Sistema emopoietico: anemia ipocromica, emorragie Sistema muscolo-scheletrico: tetania, osteomalacia S. endocrino: amenorrea, infertilità, iperparatiroidismo Cute: dermatiti Sistema nervoso: neuropatie periferiche Inquadramento fisiopatologico dei malassorbimenti 1. da difetto dei meccanismi di digestione intraluminali 2. da alterazioni primitive della mucosa intestinale 3. da riduzione della superficie assorbente 4. da ostruzione linfatica 5. da infezioni 6. da cause iatrogene o da farmaci 7. da meccanismi sconosciuti a - Deficit degli enzimi pancreatici Insufficienza del pancreas esocrino Pancreatite cronica Carcinoma del pancreas Fibrosi cistica Resezione pancreatica b - Deficit della concentrazione dei sali biliari Malattie epatiche Malattie parenchimali Colestasi intra- od extraepatica Interruzione del circolo enteroepatico della bile Da farmaci ad azione precipitante o sequestrante i sali biliari (neomicina, colestiramina) c – Iperproliferazione batterica (deconiugazione sali biliari) Stasi nella sindrome dell’ansa afferente Stenosi e atresie Fistole Ansa cieca Diverticolite multipla del tenue Sindromi da ipomobilità intestinale Da alterazioni primitive della mucosa intestinale Deficit di disaccaridasi Le disaccaridasi (lattasi, sucrasi, maltasi) sono localizzate sulla membrana delle cellule intestinali. L’assenza (congenita o acquisita) di tali enzimi provoca diarrea (osmotica) ed iperproduzione di idrogeno (per fermentazione batterica degli zuccheri non assorbiti). Non sono documentabili alterazioni al microscopio. Diagnosi di certezza: istochimica. % 2. Da alterazioni primitive della mucosa intestinale A--lipoproteinemia Malattia autosomica recessiva: difettosa sintesi di apoproteina B impossibilità al trasporto di trigliceridi a livello della mucosa intestinale; acidi grassi liberi e monogliceridi penetrano nelle cellule con funzione assorbente, ma non sono riaggregati in chilomicroni accumulo di lipidi sotto forma di vacuoli visibili al microscopio ottico; inoltre, si ha ipolipemia, con ipochilomicronemia, ipo-pre-lipoproteinemia (VLDV) e ipo-lipoproteinemia (LDL); alterazione degli eritrociti (acantociti) per difetto della struttura lipidica della membrana. %2. Da alterazioni primitive della mucosa intestinale Malassorbimento di vitamina B12 Disfunzione o resezione ileale Perdita di cellule parietali (anemia perniciosa) % 2 - Da alterazioni primitive della mucosa intestinale Cistinuria (autosomica recessiva; eccessiva eliminazione urinaria di AA dibasici a livello del tubulo prossimale renale e del digiuno aminoaciduria, malassorbimento) Amiloidosi (soprattutto associata a malattia immunocitica) Enterite eosinofila (a possibile patogenesi allergica) 3. Da riduzione della superficie assorbente del tenue Enteropatia da glutine (morbo celiaco): Malattia intestinale cronica caratterizzata da deficit dell’assorbimento intestinale, legata ad intolleranza per la gliadina ed altre proteine associate al frumento. Colpisce quasi esclusivamente la razza bianca. Casi in Europa 1: 2.000-3.000. Eziopatogenesi Ipersensibilità al glutine, contenuto nel frumento, che contiene una proteina (gliadina) solubile in alcool ed insolubile in acqua, presente nel grano, nell’orzo, nella segale e nell’avena. Probabile meccanismo: suscettibilità genetica alla gliadina e lesione intestinale immunomediata Il contatto con la gliadina provoca accumulo di linfociti B sensibilizzati verso la gliadina. Sono presenti anche anticorpi anti-gliadina in circolo. Possibile cross-reattività tra la gliadina ed una proteina dell’adenovirus tipo 12 (possibile fattore ambientale in aggiunta a quello genetico). DIGIUNO Mucosa normale Morbo celiaco The small intestinal mucosa at high magnification shows marked chronic inflammation in celiac sprue. There is sensitivity to gluten, which contains the protein gliaden, found in cereal grains wheat, oats, barley, and rye. Removing foods containing these grains from the diet will cause this gluten-sensitive enteropathy to subside. The enteropathy shown here has loss of crypts, increased mitotic activity, loss of brush border, and infiltration with lymphocytes and plasma cells (B-cells sensitized to gliaden). 3. Da riduzione della superficie assorbente del tenue Morbo di Crohn ma anche per: interruzione del circolo enteroepatico biliare iperproliferazione batterica diminuita funzione assorbente ipoproteinemia ( funzione pancreatica) Enteriti diffuse associate a linfoma 4 Da ostruzione linfatica Linfomi intestinali primitivi ma anche per interessamento mucoso diffuso stenosi iperproliferazione batterica Morbo di Whipple Tubercolosi Linfangectasie Morbo di Whipple Malattia rara (maschi adulti, 30-60 anni), a carattere sistemico, con manifestazioni intestinali, responsabili di diarrea cronica e malassorbimento, e coinvolgimento di cute, SNC, cuore, vasi, polmoni, reni, sierose, linfonodi, milza e fegato. Altri segni: poliartrite migrante, disturbi neurologici, versamenti pleurici, linfoadenopatie, febbre. Eziologia probabilmente batterica: microrganismi bastoncelliformi nella tonaca propria, extra- ed intracellulari macrofagi. All’interno di questi, glicoproteine PAS-positive, possibile prodotto batterico. Microrganismi isolati: oltre 25 tipi. La malattia risponde alla terapia antibiotica. Diagnosi: biopsia duodenale o digiunale. Abnormal small intestinal mucosa. Villli are short and flattened (yellow arrow). This is seen in malabsorption syndromes Celiac disease is a genetic, immunologically mediated small bowel enteropathy that causes malabsorption. The immune inflammatory response to gluten frequently causes damage to many other tissues of the body. The condition is frequently underdiagnosed because of its protean presentations. New prevalence data indicate that symptomatic and latent celiac disease is present in one of 300 people of European descent. Age of onset ranges from infancy to old age. Symptomatic presentations include general ill-health, as well as dermatologic, hematologic, musculoskeletal, mucosal, dental, psychologic and neurologic diseases. Celiac disease has a 95 percent genetic predisposition and, thus, it is frequently associated with autoimmune conditions such as diabetes mellitus type 1 and thyroid disease. Untreated patients have an increased incidence of osteoporosis and intestinal lymphoma. Excellent diagnostic screening tests are now available, including those that detect antigliadin and antiendomysial antibodies. Therapy with a gluten-free diet is effective, resulting in complete resolution of symptoms and secondary complications in almost all patients. Local and national celiac-sprue associations facilitate care of patients with celiac disease and support dietary compliance. Celiac disease is a gluten enteropathy occurring in both children and adults. The condition is characterized by a sensitivity to gluten that results in inflammation and atrophy of the mucosa of the small intestine. Clinical manifestations include malabsorption with symptoms of diarrhea, steatorrhea, and nutritional and vitamin deficiencies. Secondary immunologic illnesses, such as atopic dermatitis, dermatitis herpetiformis, alopecia and aphthous ulcers, may be the primary presentation PATOGENESI The immune system is abnormally activated by gluten, specifically the gliadin portion of wheat protein, and prolamines (insoluble proteins) in rye, barley and oats. Thus, celiac disease is a genetic, immunologically mediated, small intestine enteropathy in which mucosal villi are destroyed by cellular and humoral-mediated immunologic reactions to gliadin protein. The loss of functioning villi limits the ability of the small intestine to absorb nutrients, thus adversely affecting all systems of the body. The immunologic response to gluten may also occur secondarily in other bodily tissues, an example being dermatitis herpetiformis. Strong association with specific HLA class II genotypes. Approximately 95 percent of patients with celiac disease have a particular type of HLA DQ alpha and beta chain encoded by two genes, HLA-DQA1 0501 and HLA-DQB1 0201. If people genetically predisposed to celiac disease do not ingest gluten, they have no manifest illness. Delaying ingestion of gluten products through breast feeding or dietary habits may change or delay the onset of disease. Viral exposures may trigger an immunologic response in persons genetically susceptible to celiac disease; this occurs with adenovirus type 12, which shares a sequence of eight to 12 amino acids with the toxic gliadin fraction PRESENTAZIONE CLINICA During the first year of life, an infant may manifest celiac disease with intermittent vomiting, diarrhea, growth delay and failure to thrive. The incidence of this early classic presentation in infants has decreased. Children with celiac disease may present with short stature, anemia, hepatitis, epilepsy and other extragastrointestinal conditions. With age, these presentations become more subtle: the most frequent symptoms being abdominal pain, aphthous stomatitis and atopic dermatitis Giovani adulti: The initial presentation of celiac disease in patients in their 20s and 30s may be dermatitis herpetiformis. This condition usually appears as clear or blood-tinged vesicles symmetrically distributed over the extensor areas of the elbows, knees, buttocks, shoulders and scalp. Intense pruritus and/or burning sensations in the area occur hours before the onset of the vesicle. Dermatitis herpetiformis flares after consumption of foods containing a high amount of gluten Adults Malabsorption. The varied signs and symptoms of malabsorption may be caused by celiac disease or many other diseases. Mild malabsorption may be asymptomatic. With its gradual onset, the classic manifestations of flatulence and bulky, greasy and foul-smelling stools may not be recognized by the patient as signs of celiac disease. Malabsorption should be suspected in any patient with weight loss and diarrhea, and the signs and symptoms of specific vitamin or nutritional deficiencies. The latter include visual disturbances, neuropathy, anemia, osteopenic bone disease, tetany, hemorrhagic diathesis or infertility Anemia Anemia is a frequent presentation of celiac disease. Screening for occult blood in stool is considered primarily a screening for cancer, but celiac disease should be considered in the differential diagnosis Osteopenia Osteopenia may be the initial finding in patients with celiac disease. Reduced mineralization occurs in asymptomatic celiac patients, and that early diagnosis and treatment can prevent bone demineralization. Seizures There have been numerous reports of children and adults with seizures associated with celiac disease. Calcificazioni cerebrali sono una frequente complicanza. Chronic folic acid deficiency in untreated patients was considered a possible explanation Hepatic Disease. Computed tomographic scan showing occipital calcification in a patient with celiac disease and epilepsy. Celiac disease has long been recognized as a cause of chronic hepatic pathology Malattie associate: Diabete mellito di tipo I; malattie autoimmuni della tiroide Normal small intestinal mucosa is seen at the left, and mucosa involved by celiac sprue at the right. There is blunting and flattening of villi with celiac disease, and in severe cases a loss of villi with flattening of the mucosa as seen here. Celiac sprue has a prevalence of about 1:2000 Caucasians, but is rarely seen in other races. Over 95% of affected patients will express the DQw2 histocompatibility antigen, which suggests a genetic basis The small intestinal mucosa at high magnification shows marked chronic inflammation in celiac sprue. There is sensitivity to gluten, which contains the protein gliaden, found in cereal grains wheat, oats, barley, and rye. Removing foods containing these grains from the diet will cause this gluten-sensitive enteropathy to subside. The enteropathy shown here has loss of crypts, increased mitotic activity, loss of brush border, and infiltration with lymphocytes and plasma cells (B-cells sensitized to gliaden). Lactose intolerance is the inability to digest significant amounts of lactose, the major sugar found in milk. Lactose intolerance is caused by a shortage of the enzyme lactase, which is produced by the cells that line the small intestine. Lactase breaks down milk sugar into two simpler forms of sugar called glucose and galactose, which are then absorbed into the bloodstream. Not all people deficient in lactase have the symptoms commonly associated with lactose intolerance, but those who do are said to have lactose intolerance. People sometimes confuse lactose intolerance with cow’s milk intolerance because the symptoms are often the same. However, lactose intolerance and cow’s milk intolerance are not related. Being intolerant to cow’s milk is an allergic reaction triggered by the immune system. Lactose intolerance is a problem caused by the digestive system SINTOMI People who do not have enough lactase to digest the amount of lactose they consume may feel very uncomfortable when they digest milk products. Common symptoms, which range from mild to severe, include nausea, cramps, bloating, gas, and diarrhea. Symptoms begin about 30 minutes to 2 hours after eating or drinking foods containing lactose Short-bowel syndrome SBS, short gut syndrome, anenteric malabsorption syndrome, malabsorption, maldigestion, malnutrition, diarrhea, fluid disturbances, electrolyte disturbances, total parenteral nutrition, TPN The average length of the adult human small intestine has been calculated at approximately 600 cm from studies performed on cadavers. According to Lennard-Jones and to Weser (1983), this figure ranges from 260-800 cm. Any disease, traumatic injury, vascular accident, or other pathology that leaves less than 200 cm of viable small bowel places the patient at risk for developing short-bowel syndrome The short-bowel syndrome is a disorder clinically defined by malabsorption, diarrhea, fluid and electrolyte disturbances, and malnutrition. The final common etiologic factor in all causes of short-bowel syndrome is the functional or anatomic loss of extensive segments of small intestine so that absorptive capacity is severely compromised. Although resection of the colon alone typically does not result in short-bowel syndrome, its presence or loss can be a critical factor in the management of patients who lose significant amounts of small intestine. Massive small intestinal resection compromises digestive and absorptive processes. Adequate digestion and absorption cannot take place, and proper nutritional status cannot be maintained without supportive care. Examples of clinical conditions that can result in the short-bowel syndrome include mesenteric ischemia, trauma, inflammatory bowel disease, cancer, radiation enteritis, congenital short small bowel, midgut volvulus, multiple small bowel atresias, gastroschisis, meconium peritonitis, and necrotizing enterocolitis. Not all patients with loss of significant amounts of small intestine develop the short-bowel syndrome. Important cofactors that help to determine whether the syndrome will develop or not include the premorbid length of small bowel, the segment of intestine that is lost, the age of the patient at the time of bowel loss, the remaining length of small bowel and colon, and the presence or absence of the ileocecal valve. DISSENTERIA SHIGELLA, ENTAMOEBA HISTOLYTICA Dysentery - bloody diarrhoea - is one of the most dangerous types of diarrhoea. In general. it is more severe and more likely to result in death than other forms of acute diarrhoea. Other symptoms can include abdominal cramps, fever, or severe pain during defecation Large scale outbreaks (epidemics) of dysentery are a particular threat to public health. The death rate can be as high as 15 per cent, and health care services are severely stretched during epidemics. Even when correctly treated, about 5 per cent of people with dysentery can die during an epidemic. The bacterium responsible for epidemic dysentery is Shigella dysenteriae type 1 (Sd1 ) (1). S. dysenteriae is one of four species of Shigella. The others are Shigella flexneri, Shigella sonnei and Shigella boydii. These species are usually less dangerous than Sd1 and they do not cause large epidemics. Disease caused by Sd1 tends to be more common in infants, and elderly and malnourished people. Mortality is also highest in these groups. Since Sd1 was first identified late last century, extensive epidemics have been reported in Africa, Asia and Latin America. An epidemic of Sd1 in Latin America between 1969 and 1973 was responsible for more than 500,000 cases of dysentery and 20,000 deaths Altre cause di dissenteria: The most severe episodes of endemic dysentery are caused by other species of Shigella - Shigella flexneri, Shigella boydii and Shigella sonnei. Other pathogens causing endemic dysentery in children include: Campylobacter jejuni, invasive strains of Escherichia coli, non-typhoid Salmonella strains and Entamoeba histolytica Shigellosis is a bacterial infection affecting the intestinal tract. It is a fairly common disease; 600-800 cases occur in New York State each year. Most cases are seen in the summer and early fall and occur as single cases or outbreaks It is recognized more often in young children. Those who may be at greater risk include children in daycare centers, foreign travelers to certain countries, institutionalized people and active homosexuals Shigella germs are found in the intestinal tract of infected people, and is spread by eating or drinking food or water contaminated by an infected person. It can also be spread by direct contact with an infected person Sintomi: People exposed to the shigella germ may experience mild or severe diarrhea, often with fever and traces of blood or mucous in the stool. Some infected people may not show any symptoms The symptoms may appear one to seven days after exposure but usually within two to three days DIARREA Diarrhea—loose, watery stools occurring more than three times in one day— is a common problem that usually lasts a day or two and goes away on its own without any special treatment. However, prolonged diarrhea can be a sign of other problems. People with diarrhea may pass more than a quart of stool a day. Diarrhea can cause dehydration, which means the body lacks enough fluid to function properly. Dehydration is particularly dangerous in children and the elderly, and it must be treated promptly to avoid serious health problems Diarrhea may be caused by a temporary problem, like an infection, or a chronic problem, like an intestinal disease. A few of the more common causes of diarrhea are: Bacterial infections. Several types of bacteria, consumed through contaminated food or water, can cause diarrhea. Common culprits include Campylobacter, Salmonella, Shigella, and Escherichia coli. Viral infections. Many viruses cause diarrhea, including rotavirus, Norwalk virus, cytomegalovirus, herpes simplex virus, and viral hepatitis. Food intolerances. Some people are unable to digest some component of food, such as lactose, the sugar found in milk. Parasites. Parasites can enter the body through food or water and settle in the digestive system. Parasites that cause diarrhea include Giardia lamblia, Entamoeba histolytica, and Cryptosporidium. Reaction to medicines, such as antibiotics, blood pressure medications, and antacids containing magnesium. Intestinal diseases, like inflammatory bowel disease or celiac disease. Functional bowel disorders, such as irritable bowel syndrome, in which the intestines do not work normally Some people develop diarrhea after stomach surgery or removal of the gallbladder. The reason may be a change in how quickly food moves through the digestive system after stomach surgery or an increase in bile in the colon that can occur after gallbladder surgery. ALTRI SINTOMI Diarrhea may be accompanied by cramping abdominal pain, bloating, nausea, or an urgent need to use the bathroom. Depending on the cause, a person may have a fever or bloody stools Diarrhea can be either acute (short-term) or chronic (long-term). The acute form, which lasts less than 4 weeks, is usually related to a bacterial, viral, or parasitic infection. Chronic diarrhea lasts more than 4 weeks and is usually related to functional disorders like irritable bowel syndrome or inflammatory bowel diseases like celiac disease Children can have acute or chronic forms of diarrhea. Causes include bacteria, viruses, parasites, medications, functional disorders, and food sensitivities. Infection with the rotavirus is the most common cause of acute childhood diarrhea. Rotavirus diarrhea usually resolves in 3 to 9 days General signs of dehydration include: thirst, less frequent urination, dry skin, fatigue, light-headedness dark colored urine Signs of dehydration in children include dry mouth and tongue no tears when crying no wet diapers for 3 hours or more sunken abdomen, eyes, or cheeks high fever listlessness or irritability skin that does not flatten when pinched and released Yellow arrow depicts crescent shaped trophozoite, while the red arrow depicts a teardrop shaped trophozoite of giardia This is an example of infectious diarrhea due to Giardia lamblia infection of the small intestine. The small pear-shaped trophozoites live in the duodenum and become infective cysts that are excreted. They produce a watery diarrhea. A useful test for diagnosis of infectious diarrheas is stool examination for ova and parasites Cryptosporidiosis -- Small spherical organisms (red arrow) attached to the brush border of absorptive intestinal epithelial cells. This is another infectious agent that is becoming more frequent in immunocompromised patients, particularly those with AIDS. The small round blue organisms at the lumenal border are cryptosporidia. Cryptosporidiosis produces a copious watery diarrhea VIRUS CAUSA DI DIARREA Astrovirus; calicivirus; reovirus (rotavirus; “picorna/enterovirus”) Reovirus: Respiratory Enteric Orphan viruses, i.e. infect the human respiratory and intestinal tracts, usually without disease symptoms One well documented source of infection is the consumption of shellfish (polluted by sewage) - and therefore, they also have economic consequences for fishermen and the food industry. Such viruses often cause mini-epidemics in families, hospital wards, etc and are potentially very dangerous to seriously ill hospital patients. More importantly, these viruses contribute to the massive mortality caused by infantile diarrhoea in developing countries and are responsible for uncounted millions of deaths each year. Cause di diarrea severa/morte COLERA Cholera is an acute intestinal infection caused by ingestion of food or water contaminated with the bacterium Vibrio cholerae. It has a short incubation period, from less than one day to five days, and produces an enterotoxin that causes a copious, painless, watery diarrhoea that can quickly lead to severe dehydration and death if treatment is not promptly given. Vomiting also occurs in most patients. Most persons infected with V. cholerae do not become ill, although the bacterium is present in their faeces for 7-14 days. When illness does occur, more than 90% of episodes are of mild or moderate severity and are difficult to distinguish clinically from other types of acute diarrhoea. Less than 10% of ill persons develop typical cholera with signs of moderate or severe dehydration. BACKGROUND The vibrio responsible for the seventh pandemic, now in progress, is known as V. cholerae O1, biotype El Tor. The current seventh pandemic began in 1961 when the vibrio first appeared as a cause of epidemic cholera in Celebes (Sulawesi), Indonesia. The disease then spread rapidly to other countries of eastern Asia and reached Bangladesh in 1963, India in 1964, and the USSR, Iran and Iraq in 1965-1966. In 1970 cholera invaded West Africa, which had not experienced the disease for more than 100 years. The disease quickly spread to a number of countries and eventually became endemic in most of the continent. In 1991 cholera struck Latin America, where it had also been absent for more than a century. Within the year it spread to 11 countries, and subsequently throughout the continent. Until 1992, only V. cholerae serogroup O1 caused epidemic cholera. Some other serogroups could cause sporadic cases of diarrhoea, but not epidemic cholera. Late that year, however, large outbreaks of cholera began in India and Bangladesh that were caused by a previously unrecognized serogroup of V. cholerae, designated O139, synonym Bengal. Isolation of this vibrio has now been reported from 11 countries in South-East Asia. It is still unclear whether V. cholerae O139 will extend to other regions, and careful epidemiological monitoring of the situation is being maintained. TRASMISSIONE Cholera is spread by contaminated water and food. Sudden large outbreaks are usually caused by a contaminated water supply. Only rarely is cholera transmitted by direct person-to-person contact. In highly endemic areas, it is mainly a disease of young children, although breastfeeding infants are rarely affected. Vibrio cholerae is often found in the aquatic environment and is part of the normal flora of brackish water and estuaries. It is often associated with algal blooms (plankton), which are influenced by the temperature of the water. Human beings are also one of the reservoirs of the pathogenic form of Vibrio cholerae Man-made and natural disasters can intensify the risk of epidemics considerably, as can conditions in crowded refugee camps. Explosive outbreaks with high case-fatality rates are often the result. For example, in the aftermath of the Rwanda crisis in 1994, outbreaks of cholera caused at least 48 000 cases and 23 800 deaths within one month in the refugee camps in Goma, the Congo. Although rarely so deadly, outbreaks continue to be of major public health concern, causing considerable socioeconomic disruption as well as loss of life. In 2001 alone, WHO and its partners in the Global Outbreak Alert and Response Network participated in the verification of 41 cholera outbreaks in 28 countries The small intestinal mucosa demonstrates marked hyperemia as a result of ischemic enteritis. Such ischemia most often results from hypotension (shock) from cardiac failure, from marked blood loss, or from loss of blood supply from mechanical obstruction (as with the bowel incarcerated in a hernia or with volvulus or intussusception). If the blood supply is not quickly restored, the bowel will infarct On closer inspection, early ischemic enteritis involves the tips of the villi. A colonoscopic view of ischemic colitis with minimal overlying exudate is shown below. In general, bowel is hard to infarct from atherosclerotic vascular narrowing or thromboembolization because of the widely anastomosing blood supply. Thus, most cases of bowel ischemia and infarction result from generalized hypotension and decreased cardiac output The mucosal surface of the bowel seen here shows early necrosis with hyperemia extending all the way from mucosa to submucosal and muscular wall vessels. The submucosa and muscularis, however, are still intact At higher magnification with more advanced necrosis, the small intestinal mucosa shows hemorrhage with acute inflammation in this case of ischemic enteritis The dark red infarcted small intestine contrasts with the light pink viable bowel. The forceps extend through an internal hernia in which a loop of bowel and mesentery has been caught. This is one complication of adhesions from previous surgery. The trapped bowel has lost its blood supply. This is normal colonic mucosa. Note the crypts that are lined by numerous goblet cells. In the submucosa is a lymphoid nodule. The gut-associated lymphoid tissue as a unit represents the largest lymphoid organ of the body Typical pseudomembranes adherent to the colonic mucosa in antibiotic-associated colitis. The illness occurs after a course of broad-spectrum antibiotics, which permit overgrowth of the bacteria Clostridium difficile. This is an example of pseudomembranous enterocolitis. The mucosal surface of the colon seen here is hyperemic and is partially covered by a yellow-green exudate. The mucosa itself is not eroded. Broad spectrum antibiotic usage (such as clindamycin) and/or immunosuppression allows overgrowth of bacteria such as Clostridium dificile or S. aureus or fungi such as Candida to cause this appearance. The colonoscopic appearance is seen below This is another example of pseudomembranous inflammation, this time in the ileum. A greenish-yellow exudate covers most of the mucosal surface Microscopically, the pseudomembrane is seen to be composed of inflammatory cells, necrotic epithelium, and mucus in which the overgrowth of microorganisms takes place. The underlying mucosa shows congested vessels, but is still intact At higher magnification, the overlying pseudomembrane at the left has numerous inflammatory cells, mainly neutrophils Left: Hypervascularity of the rectal mucosa in a 65 year-old man who had previously undergone radiation therapy for carcinoma of the prostate. Center: Close-up of vascular ectasias of the rectal mucosa following radiation therapy for prostatic carcinoma in a 75 year-old man. Right: Post-irradiation mucosal vascular changes in a 73 year-old woman with rectal bleeding. 24 year-old with bloody diarrhea. Sigmoidoscopy revealed mucosal inflammation with erythema (redness), edema (swelling), granularity and loss of the normal vascular pattern. Stool culture grew Salmonella. 34 year-old man, infected with HIV, who presented with diarrhea. Sigmoidoscopy revealed mucosal inflammation with focal mucosal hemorrhage, edematous folds and polypoid lesions. Biopsies demonstrated viral inclusions consistent with cytomegalovirus 70 year-old woman with AIDS, whose symptoms included diarrhea. At colonoscopy, a large, deep U-shaped ulcer was found in the cecum (left). A second ulcer was seen in the rectum at retroflexion (center). Biopsies were consistent with cytomegalovirus infection. Extensive ulceration in the poorly prepped colon of a 33 year old man with AIDS (right), who had presented with colonic pseudo-obstruction. Biopsies demonstrated CMV 72 year-old woman who presented with abdominal pain, bloody diarrhea and weight loss. She had been taking significant amounts of nonsteroidal antiinflammatory agents (NSAIDs) for arthritis. Colonoscopy revealed segmental mucosal inflammation with ulceration. Although grossly similar in appearance to ischemic colitis, the typical histological features of ischemic colitis (mucosal necrosis, fibrosis of the lamina propria and crypt atrophy, and overlying fibrinopurulent membrane) were not present on biopsy. 44 year-old man, a frequent user of cocaine, who presented with bloody diarrhea. Colonoscopy revealed a range of findings from areas of congestion (upper right) to sessile polyps (upper left) to lesions resembling pedunculated polyps (lower left). Stool cultures were all negative. Biopsies revealed mucosal congestion and inflammation. The tips of the more polypoid lesions showed severe ischemia histologically Colonoscopy, Enterobius Vermicularis (pinworms) – Endoscopy reveals an area of mucosal erythema a white "s" shaped organism with features of e. vermicularis Pinworms (Enterobiasis vermicularis) -- Intestinal lumen containing a cross section of an adult e. vermicularis demonstrating a central intestine of the worm (yellow arrow) and lateral ala (red arrow).
Scarica